Sep 3, 2020
You may have seen stories in the news about the potential of cell therapy to treat severe cases of COVID-19. One story in particular mentioned positive results of an experimental study of stem cells with the patient mortality rate decreasing from 85 percent to 15 percent.[i] Stem cell therapy has been shown to have regenerative, anti-inflammatory and immunomodulating properties. Although this patient sample was very small, this is yet another reminder that cell therapy has moved to the forefront of medicine.
Bone marrow transplantation for blood diseases has been in use for more than 40 years[ii], but more recently has been used to treat orthopedic injuries including joint degeneration and pain.
Why Do My Joints Hurt?
It is not uncommon to experience pain in the shoulders, elbows, knees or hips. Sometimes even the toe joints can hurt. Whether big or small, painful joints can make daily activities difficult and significantly impact your quality of life.
Pain in the joints may result from several different conditions. These include:
· Osteoarthritis: a condition that develops when the cartilage in the joints begins to break down. It often occurs as a result of trauma, aging, obesity or genetic factors.
· Tears or sprains to soft tissues surrounding the joint such as muscles, tendons and ligaments.
· Chronic inflammation due to autoimmune diseases such as lupus or rheumatoid arthritis.
The good news is that cell therapies that use a patient’s own blood, bone marrow or adipose (fat tissue) have proven to be effective at treating joint pain without surgery or extended rehabilitation.
Fat Cells or Bone Marrow Cells?
Cell therapy is derived from two major sources of cells, adipose (fat) cells and bone marrow cells. Each can be easily obtained in the clinic, but the two offer different healing properties.
Adipose-derived cells are taken from the abdomen, flank or thighs. These cells can repair and replace damaged or injured tissue. The specialized healing cells are called pericytes and they direct other cells to form new blood vessels, awaken stem cells and stimulate the growth of new tissues such as cartilage, bone and tendon. They also secrete powerful anti-inflammatory and pain relieving molecules.
Bone marrow cells can be used for injury recovery and more rapid healing. That’s because bone marrow contains cells that have the ability to improve circulation, decrease inflammation and regenerate healthy tendons, ligaments and cartilage.
How Effective is Cell Based Therapy?
Like all medical treatments, outcomes are significantly impacted by several factors, including:
· The extent of the damage being treated.
· The patient’s overall health prior to the procedure.
· How the orthobiologics are prepared for treatment.
· For many patients, however, using adipose and bone marrow cells to treat orthopedic injuries is highly effective and does not present many of the risks associated with traditional invasive surgery.
The procedure is performed on an out-patient basis in the physician’s office. Most patients require only a single treatment and many are able to resume their normal activities within days.
San Diego Orthobiologics Medical Group is one of only six clinics in the U.S. to participate in a first-of- its-kind FDA-approved clinical trial to treat knee osteoarthritis using a patient’s own fat-derived stem cells.
Drs. Christopher Rogers and Mary Ambach of San Diego Orthobiologics Medical Group were chosen based on their extensive experience with cell therapy to treat orthopedic conditions.
Sources:
[i] News – Medical: Study: Cellular Therapy Can Improve Severe Cases of COVID-19
[ii] Hopkins Medicine: Research: Cell Therapy

Aug 28, 2020
The liquid portion of blood called plasma has been used for several years to help patients facing life-threatening conditions such as immune deficiency disorders and organ transplantation. Because it has helped treat so many chronic and rare diseases, it has been referred to as “the gift of life.”[i]
More recently, physicians have discovered that a patient’s own plasma and its’ cells can help expedite the recovery from orthopedic injuries. Platelet rich plasma treatments, known as PRP, use the healing power of platelets to harness growth factors and other proteins that are essential for healing.
How Platelet Rich Plasma Treatment Works
Blood is comprised of red blood cells, white blood cells,platelets and plasma. The plasma contains hormones, electrolytes and nutrients that are needed to nourish cells during the healing process.
During platelet rich plasma treatment, the patient’s own blood is drawn and placed in a centrifuge machine where the platelets are separated and concentrated. This results in a PRP solution that contains up to 10 times more platelets than that typically found in blood.[ii] With its super-charged healing capabilities, platelet rich plasma can be used to treat a number of orthopedic conditions, including:
· Joint arthritis (knee, shoulder, hip, thumb or spine)
· Injured tendons like rotator cuff tendon, Tennis elbow and Achilles tendon
· Ligament sprains in the wrist, ankle or sacroiliac joints
· Carpal tunnel syndrome
· Degenerated discs, mild spinal stenosis and sciatica
Not All PRP Treatments Are the Same
When it comes to platelet rich plasma treatment, one size does not fit all. Several factors can influence the success rate of treatment:
· The patient must receive an accurate diagnosis.
· Image guidance with ultrasound or fluoroscopy (x-ray) for targeted delivery to the injured tissues is necessary.
· The PRP formulation must be customized to the specific injury being treated.
· The initial injury severity must be considered.
When administered appropriately and in the right formulation for the specific injury, most patients begin to experience results within four to eight weeks after platelet rich plasma treatment. About 10% of patients will feel relief within days.
PRP treatments are performed on an out-patient basis in the physician’s office. There is no need for hospitalization or lengthy rehabilitation. The entire procedure takes less than an hour and patients may typically resume normal activity within days.
Dr. Christopher Rogers of San Diego Orthobiologics Medical Group performed one of the first PRP treatments in San Diego in 2009. He and Dr. Mary Ambach are experts in the field of regenerative therapy for orthopedic injuries. They have successfully treated thousands of patients with PRP and other orthobiologics.
Sources:
[i] Donating Plasma: What is Plasma
[ii] OrthoInfo: Platelet Rich Plasma

Aug 19, 2020
Pain and stiffness due to arthritis has long been considered something that normally comes with age. But new research indicates that the disease has affected younger people too at an increasing rate. The Arthritis Foundation reported that among those aged 18 to 64, nearly one in three have doctor-diagnosed arthritis and/or report joint symptoms consistent with a diagnosis of arthritis in both men and women.[i]
Osteoarthritis occurs when the cartilage that cushions the bones in the joints begins to break down. This is often a result of life-long wear and tear, but overuse from repetitive motions and activities may lead to earlier development of this painful condition.
Are You at Risk for Developing Osteoarthritis?
The odds of developing osteoarthritis increase with age and repetitive use, but there are several other factors that can increase a person’s risk for joint degeneration including:
- Genetics: Some people inherit a tendency to develop osteoarthritis.
- Gender: Women are more likely to develop osteoarthritis than men for ill-defined reasons.
- Obesity: Extra pounds put stress on weight-bearing joints, such as your hips and knees.
- Previous Injury: Joints injured by an accident or surgery, are more prone to developing osteoarthritis.
- Other medical conditions: Systemic diseases such as diabetes and hemochromatosis (a condition that causes the body to retain too much iron) are at higher risk too.
Addressing the Pain Without Surgery
The field of regenerative medicine has made great strides in the development of non-surgical treatments for patients suffering with painful joints due to osteoarthritis. These treatments use a patient’s own cells and tissues to stimulate the body’s ability to repair damaged joints and encourage the growth of new tissue, such as cartilage, bone and tendon.
These minimally-invasive treatments are performed using advanced image guidance to deliver cellular therapy to the affected areas with high precision. They are performed in the medical clinic allowing patients to return home within an hour or two of their treatment.
Such innovative therapies include:
- Prolotherapy which stimulates the body’s natural healing mechanisms to produce new tissue by employing a sugar based solution called dextrose.
- Platelet Rich Plasma (PRP) therapy that selectively concentrates platelets and growth factors in the blood to create a customized healing treatment.
- Bone Marrow Aspiration Concentrate (BMAC) which uses stem cells, platelets and other substances in the patient’s bone marrow that improve circulation, decrease excessive inflammation and regenerate healthy tissue.
- Lipogems that enables cells within the adipose (fat) tissue to work together as a functional unit and repairs, reconstructs and replaces damaged tissues.
- Master Protease Inhibitor (Alpha 2 Macroglobulin or A2M) which uses a substance found in a patient’s own blood to stop the progression of joint degeneration and decrease inflammation.
Which Treatment is Right for Me?
Arthritis sufferers who are considering regenerative treatments should consult with a qualified physician who has the training and skills to perform these procedures safely and effectively. These physicians are board-certified in physical medicine and rehabilitation (PM&R), sports medicine or orthopedics and have advanced training in regenerative medicine. They can help you determine which treatment is most appropriate based on your goals and specific medical condition.
Another important factor to consider is the source of the regenerative products. Practices that use autologous cells and tissue from a patient’s own body are permitted by the FDA when used in accordance with their guidelines. Clinics that use donor birth tissue products, such as umbilical cord blood, amniotic fluid or exosomes put their patients at risk for infection or immune reactions because these materials are foreign to a patient’s own body. The FDA does not permit the use of such products because they have not been proven to be safe or effective.
Those who once considered joint replacement surgery as their only option to manage the pain of osteoarthritis should carefully review these new regenerative treatment options. They can offer years of pain relief that can delay or even avoid surgery.
Drs. Christopher J. Rogers and Mary A. Ambach are recognized experts and leaders in the field of regenerative medicine. They have published in the scientific literature and have trained hundreds of physicians at medical conferences around the world. Because of their extensive knowledge of treating orthopedic conditions with regenerative procedures, San Diego Orthobiologics Medical Group is one of only six clinics in the United States selected to participate in an FDA-approved clinical trial to treat knee osteoarthritis with stem cells.
Sources:
[i] Arthritis By the Numbers
Jun 10, 2020
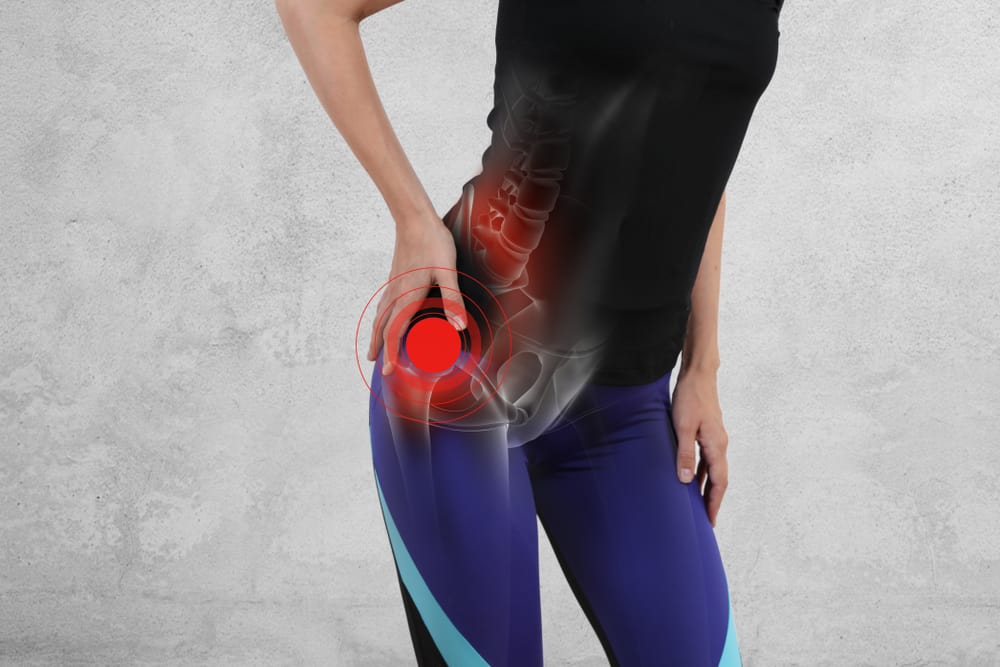
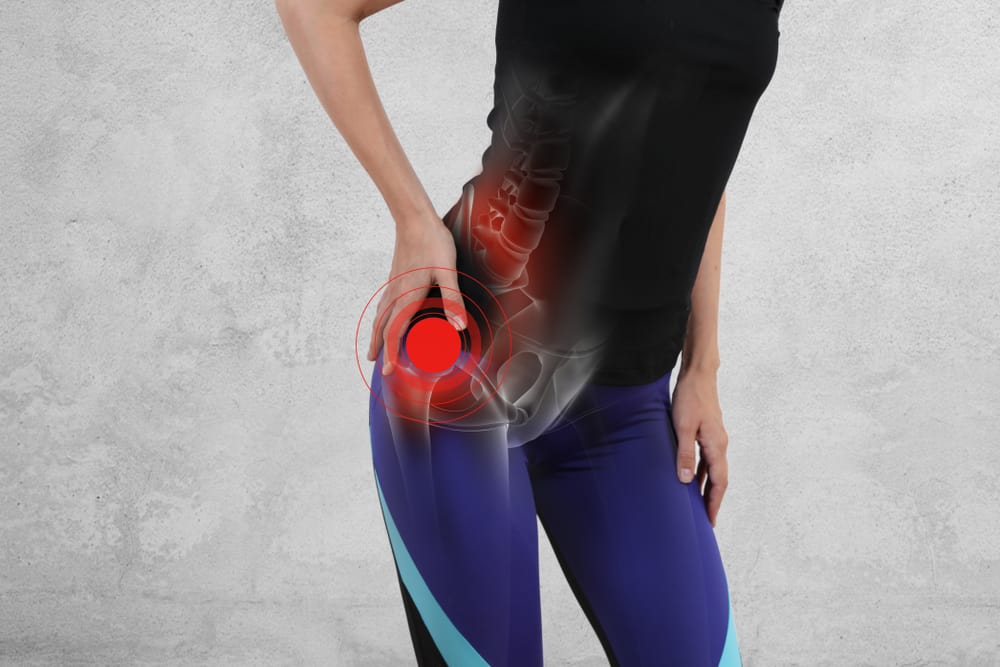
As one of the body’s largest joints, the hip gets its fair share of wear-and-tear over the years. The hip joint is a ball-and-socket joint, consisting of the femoral head at the top of the thighbone (ball) and the acetabulum in the pelvis bone (socket).
Chronic hip pain often develops in those over the age of 50, but can occur earlier, especially in those who are overweight or who have had a previous hip injury or surgery. Some people are born with abnormalities of the joint that put them at higher risk for hip issues as well.
Common symptoms of hip problems include:
- Groin pain
- Limping
- Decreased range of motion and stiffness
- Tenderness around the front or back of the hip
- Clicking, popping or locking of the joint
Why Do I Have Chronic Hip Pain?
Common causes of hip pain include:
- Osteoarthritis: chronic degeneration of the cartilage and inflammation of the hip tissues and joint fluid. The degeneration can be accelerated by trauma causing damage to the cartilage and subtle irregularities in how the hip developed in childhood.
- Bursitis: inflammation of the bursa, a fluid-filled sac that cushion the tendons overlying the bones
- Tendinitis and tendon tears: damage to the tendons in the hip, often from overuse or muscle weakness
- Labral tears: injury to the labrum, a soft cartilage tissue that surrounds the hip socket
- Sacroiliitis: Inflammation of the sacroiliac joints where your lower spine and pelvis connect.
- Avascular necrosis: impaired blood flow to the hip bone causes damage
The good news for patients suffering from chronic hip pain is that advances in regenerative medicine are giving hope to those who feared that total joint replacement therapy was their only option.
San Diego Orthobiologics Medical Group offers several advanced regenerative therapies for hip joint pain:
- Platelet Rich Plasma Therapy uses growth factors from the platelets in the patient’s own blood by releasing substances called growth factors concentrates platelets to stimulate tissue healing for degenerative joints and soft tissue injuries.
- ENDORET PRGF (platelet rich in growth factors) contains proteins that stimulate the tissue repair processes, including new blood vessel formation, cell mobilization and cell proliferation. PRGF can accelerate healing and minimize inflammation that reduces pain.
- Bone Marrow Aspirate Concentrate (BMAC): utilizes your own bone marrow which contains cells that have the ability to improve circulation, decrease inflammation and promote healing in tendons, ligaments and cartilage. BMAC provides highly concentrated regenerative cells to support a robust healing response through a simple office procedure.
- LIPOGEMS® is an FDA-compliant device for processing and same-day use of your own adipose tissue (fat) to treat joint and tendon injuries. Adipose tissue is a rich source of adipose derived stem cells and other regenerative orthobiologics.
- Prolotherapy, also known as “proliferative therapy,” delivers dextrose and other medications to help regenerate tissue and stimulate a healing response in a chronically injured ligament, tendon or joint. Prolotherapy is often combined with PRP therapy to expedite healing.
- Alpha 2 Microglobulin (A2M) uses uses orthobiologics from a patient’s own blood to stop the progression of joint degeneration, decrease inflammation and promote tissue healing.
These treatments offer better safety than most surgical procedures as they are minimally invasive and are performed in our office procedure suite. Patients do not require hospitalization, or a lengthy recovery. Many patients are able to resume normal activities within days of their treatment and see pain relief within weeks.
Drs. Christopher Rogers and Mary Ambach of San Diego Orthobiologics Medical Group are leaders in the field of regenerative medicine for orthopedic conditions. They were the first in San Diego to use Lipogems® as well as ENDORET PRGF therapy for the treatment of orthopedic conditions.
Sources:
https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/
https://www.mayoclinic.org/diseases-conditions/sacroiliitis/symptoms-causes/syc-20350747
https://www.mayoclinic.org/symptoms/hip-pain/basics/causes/sym-20050684

Jun 2, 2020
What is Prolotherapy?
Prolotherapy (short for proliferative therapy) stimulates the body’s natural healing factors to strengthen and repair injured joints, ligaments and tendons. This minimally invasive procedure is used to address a number of musculoskeletal conditions including:
- Back pain due to degenerative disc disease, sacroiliac joint instability, facet joint syndrome and nerve pain
- Neck pain due to arthritis or whiplash injury
- Knee pain caused by osteoarthritis, meniscal tears or sprains
- Arm and shoulder pain as a result of arthritis, rotator cuff tendon tears, golfer’s elbow, tennis
- elbow and chronic tendonitis.
Studies have shown that 85 to 95 percent of patients with back pain experience improvement with prolotherapy. [i] Additional studies have also shown prolotherapy is successful for various ligament, tendon or joint pain/injuries, including knee arthritis. The Annals of Family Medicine reported that a randomized controlled trial of prolotherapy in patients with knee osteoarthritis resulted in clinically meaningful sustained improvement of pain, function, and stiffness.[ii]
How It Works
Prolotherapy stimulates the body’s natural healing mechanisms to produce new tissue. Using fluoroscopic (x-ray) guidance, the physician injects a mixture of local anesthetics and dextrose (a sugar-based solution) directly to the injured area. The dextrose works as an irritant to kick start the body’s natural healing response and encourages the growth of normal ligament and tendon fibers. This results in long-term healing and pain relief. In some cases, the treatment is repeated with the goal of restoring strength and stability without loss of flexibility and function. As the body heals the pain subsides, in most cases, permanently.
Prolotherapy, when used in lower concentrations, has also been shown to help with nerve pain by blocking nerve pain impulses. This can provide immediate pain relief to joint, nerve and soft tissue injuries.
For patients with advanced injury or degeneration, prolotherapy can be combined with Platelet Rich Plasma (PRP) and autologous (from the same person) adult regenerative cells to boost the regenerative process. Every formulation is specifically targeted to the patient’s unique needs.
Is Prolotherapy Safe?
In contrast to many medical treatments that may provide only temporary benefits, prolotherapy is a safe treatment that offers long-term relief.
Prolotherapy is an in-office procedure performed under local anesthetic. There is no hospitalization required, nor the need for extended rehabilitation. Most patients are able to resume their daily activities immediately. Even those who require additional treatments are likely to enjoy significant pain relief after just one treatment.
Like every other medical intervention, the success of prolotherapy can be impacted by the patient’s overall health as well as any underlying nutritional or genetic deficiencies that might make healing more difficult. It is important to talk with your doctor about the best methods to optimize your health and healing potential.
Dr. Christopher J. Rogers and Dr. Mary A. Ambach of San Diego Orthobiologics Medical Group are leaders in the field of regenerative medicine and have been performing prolotherapy with great success for decades. They serve as faculty members and lecturers at national and international medical conferences and serve on the board of directors for several regenerative medicine organizations. They have published scientific papers in the medical literature and are dedicated to excellent patient care and advancing the field of regenerative medicine.
Resources:
[i] https://prolotherapycollege.org/what-is-prolotherapy/
[ii] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3659139/

May 15, 2020
Regenerative Therapy for Chronic Back Pain
Low back pain is the fifth most common reason a patient visits their doctor. More than 90% of the population will experience at least one episode of low back pain during their lifetime. The social and economic impact of low back pain is significant and it is responsible for about 40% of missed work days in the US.
Causes of Back Pain
There are many different causes for low back pain. The pain can be acute or chronic in nature and may originate from an injury or degenerated tissues in the spine. Common causes of low back pain include:
- Back strain: This occurs when the spine is subjected to physical stress that is greater than what can be supported by the muscular and ligamentous structures. Repeated heavy lifting or sudden awkward movements can cause over-stretching or tearing of the ligaments, tendons or muscles in the spine causing pain.
- Arthritis. Osteoarthritis of the spine can lead to degeneration that is associated with the normal wear and tear of joints, discs and bones in the spine as people age. The arthritis can lead to bone spurs which result in narrowing of the space around the spinal nerves and spinal cord; a condition called spinal stenosis.
- Facet joint dysfunction: The spinal column consists of individual bones called vertebrae. They connect to one another at each level by two small facet joints. The joints promote movement and stability between the vertebral bodies. Pain occurs when the joints get inflamed or when the cartilage in the joints becomes injured or worn out.
- Bulging or Ruptured Disc: The discs are soft, gel filled structures that act as cushion or shock absorbers between the vertebral bones in your spine. The disc also connects the adjacent vertebrae together with strong fibrous tissue. When these discs become injured, they can bulge or the gel slips out and can put pressure on neighboring nerves causing pain. As people age, discs lose their hydration and wear down leading to degeneration. Degenerative discs can develop tears and collapse which causes low back pain, muscle spasm or spinal stenosis.
There are many other causes of low back pain including nerve and spinal cord problems, scoliosis, fracture and non-spine sources like tumor and kidney stones. It is important that your physician perform a comprehensive evaluation of your medical history and physical examination to give you an appropriate diagnosis for your back pain.
Non-Surgical Options for Back Pain Relief
There are hundreds of different forms of treatment for lower back pain, however no single treatment stands out as superior to any of the others. When conservative treatments fail to relieve pain, your doctor may feel compelled to consider surgery, however, the success rate of surgery is less than 60% for most causes of lower back pain and involves significant risk and recovery time. Fortunately, there are innovative, minimally invasive treatments available.
Advanced regenerative therapy may be the best solution for your back. These advanced treatments can help you heal faster. They avoid the risks and long-term complications associated with surgery and reduce pain to help you maintain an active lifestyle.
- Platelet Rich Plasma (PRP) therapy concentrates platelets, plasma and other substances found in your blood to create a customized healing treatment for degenerative facet joints, discs and nerve pain.
- Bone Marrow Aspiration Concentrate (BMAC) utilizes your own bone marrow which contains a rich reservoir of regenerative cells, multipotent stem cells and anti-inflammatory molecules designed to stimulate your body’s ability to improve circulation, decrease inflammation and regenerate tissues. This regenerative therapy can be used for disc tears, disc degeneration and facet joint arthritis.
- Master Protease Inhibitor (A2M) uses a natural substance found in your blood (Alpha 2 Macroglobulin) to stop the progression of joint degeneration and improve pain and inflammation in arthritic joints.
- Prolotherapy: Sugar containing medications that help regenerate tissue and relieve pain are injected into injured ligaments, tendons or joints to strengthen and improve stability in patients with osteoarthritis, ligament sprains, sacroiliac joint dysfunction and sports-related injuries.
Patients who have failed standard treatments or are seeking alternatives to spine surgery for neck and back pain should consider regenerative therapies. The research on the use of these therapies for certain conditions of the spine is very promising. However, much more research still needs to be completed. The doctors of San Diego Orthobiologics Medical Group contribute to advancing the science by participating in clinical trials and publishing articles on regenerative therapies for spine and other orthopedic conditions.
Advances in regenerative medicine offer new hope for long-term pain relief and improved quality of life.
San Diego Orthobiologics Medical Group is a leader in regenerative medicine therapies and offers a great variety of treatment options depending upon each patient’s unique needs. With decades of experience in the field of minimally invasive interventional treatments, Drs. Christopher J. Rogers and Mary A. Ambach are experts in the field of regenerative medicine. They serve as faculty members and lecturers at national and international medical conferences and serve on the board of directors for several national regenerative medicine organizations.