May 27, 2022
Orthobiologics is a combination of words: “ortho” refers to the body’s musculoskeletal system (muscles, bones, joints, ligaments, and tendons), and “biologics” refers to naturally derived substances used to heal parts of the body. Orthobiologic treatments can be used to harness the body’s ability to heal itself to restore or establish normal function. Within the field of orthopedics, these specific treatments hold great promise for helping patients with injuries or degeneration in the musculoskeletal system.
When joints, ligaments, tendons, or discs are damaged, it can lead to chronic pain in the:
- Lower Back
- Knees
- Hips
- Neck
- Feet and ankles
- Hands and wrists
- Elbows and Shoulders
Orthobiologics promote healing and stimulate growth of new healthy tissues. When the underlying cause is treated, pain improves or resolves.
How Do Orthobiologics Work?
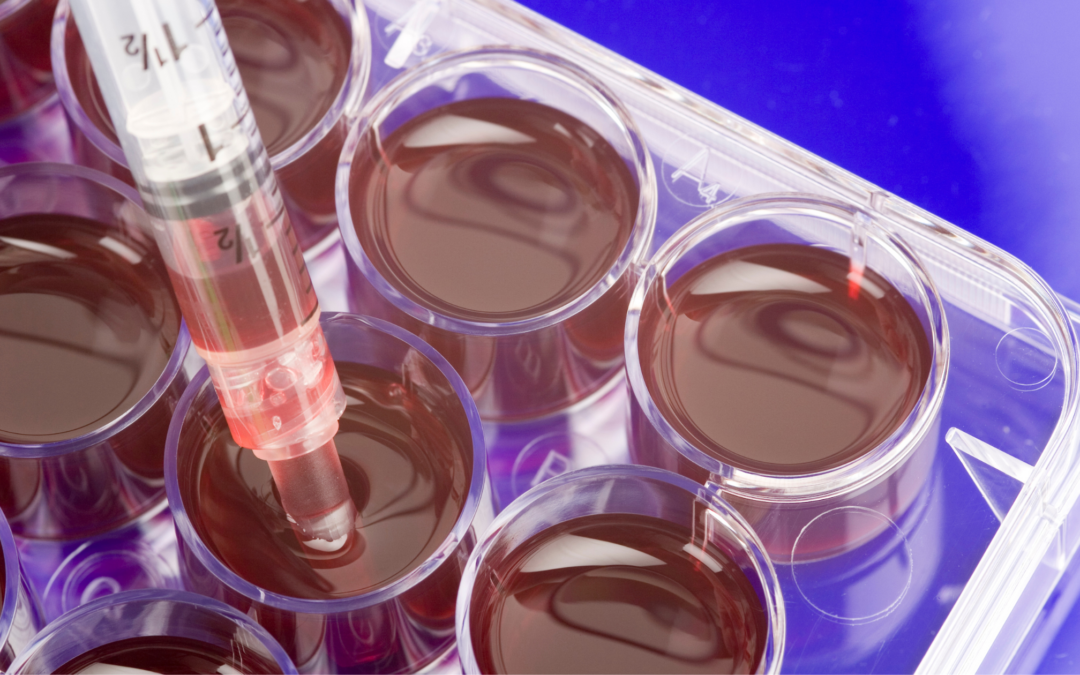
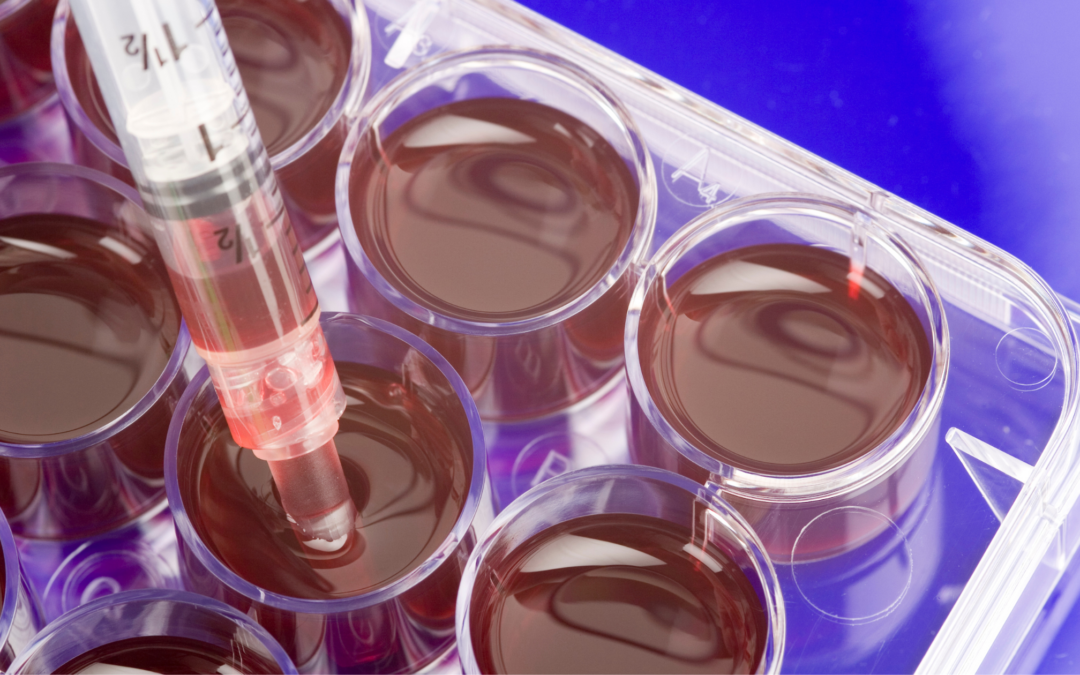
Orthobiologic treatments for orthopedic conditions use the patient’s own blood and cells (known as autologous products) to kick-start the body’s own healing processes. These biologic products are collected from the patient and concentrated to isolate the healing proteins, molecules, and nutrients they contain. These super-healers are then re-injected into the exact site of the damaged tissue to encourage new cell growth and healing.
Limitations on Cellular Treatments by the FDA
The U.S. Food & Drug Administration (FDA) does not allow the use of embryonic or blood cord products for treating orthopedic conditions. The FDA also banned certain language and vague advertising regarding these types of products that in the past have opened doors to illegal markets cell-buying and procedures that are potentially dangerous to patients.
Skilled certified physicians can use the following autologous (from your own body) cellular products to treat musculoskeletal problems, provided they follow the FDA’s guidelines for safety and efficacy:
- Platelet Rich Plasma: Platelets in the patient’s own blood release growth factors and proteins that promote tissue repair, while the plasma carries cytokines and nutrients required to nourish cells during the healing process.
- Cellular Therapies: A specific type of cells, called mesenchymal cells, taken from the patient’s own fat tissue (adipose) or bone marrow, have the unique ability to develop into the specific kind of cell needed to promote healing and possess molecules that direct other cells in the injured area to form new blood vessels, awaken other cells, and encourage newly forming cells to produce collagen and other proteins essential for creating new healthy tissues.
Because the platelet-rich plasma and mesenchymal cells are taken directly from the patient and delivered back to them, they do not present the risk of allergic reactions or some infections seen with donor products.
Are PRP and Cell Therapies Painful?
For many years, patients with unresolved chronic orthopedic pain were left to consider surgery as their best hope for long-term pain relief. But with advancements in regenerative medicine, some patients can avoid major surgery and lengthy rehab.
Orthobiologic treatments are conducted with needles. Blood plasma and mesenchymal cells are aspirated (removed via a needle) and reinjected through a needle. There are no large incisions, which means the risk of bleeding and infection is significantly reduced. It also means that the procedures can be performed on an outpatient basis, and recovery begins at home within hours of the treatment.
Best of all, patients can enjoy long-lasting pain relief and enjoy an improved quality of life without chronic pain.
Ask the Right Questions, Get the Best Results
When considering regenerative medicine to treat orthopedic conditions, patients should make sure:
- The physician performing the procedure is board-certified
- Advanced centrifuge technology is used to prepare the cellular products so that they offer the highest possible concentrations of healing properties.
- Treatments are given under fluoroscopic (X-ray) or ultrasound guidance to ensure precise delivery of the regenerative products to the exact site of the injury.
- The practice acknowledges and strictly follows FDA guidelines for the use of cellular products to treat musculoskeletal damage.
The best outcomes occur when the patient understands the benefits of regenerative treatments and knows the right questions to ask prior to the procedure.
SDOMG is a state-of-the-art practice focusing on Orthobiologics to treat orthopedic conditions. To learn more about the procedures they provide, visit their website or fill out the form below. We look forward to helping you regain your quality of life.

Jun 11, 2021
What Conditions Can Orthobiologics Treat?
The musculoskeletal system is the body’s interconnected network of bones, muscles, tendons, ligaments and connective tissues that helps you move and perform tasks of everyday living. But if injury or disease such as degenerative arthritis cause parts of the system to break down, the result can be pain, swelling, weakness and stiffness.
The good news however, is that the body has regenerative properties that we can harness to treat orthopedic injuries involving the joints and soft tissues in the back, neck, knees, hips, elbows, shoulders, wrists and ankles.
Orthobiologics are natural substances such as cells, cell molecules and tissues derived from the patient’s own body that are harnessed to stimulate healing of orthopedic injuries or conditions.
What are the different types of Orthobiologics used in clinical practice?
- Platelet Rich Plasma (PRP): Concentrated solution of platelets derived from the patient’s own blood which contain a significant amount of growth factors and proteins that promote tissue regeneration, decrease inflammation and encourage blood vessel formation.
- Cell Based Therapies: Cells taken from the patient’s own fat tissue (Microfragmented Adipose Tissue) or bone marrow (Bone marrow Aspiration Concentrate) contain adult stem cells that have the unique ability to renew themselves and develop into other cell types. They promote tissue healing, control inflammation and fight infection.
Do Orthobiologics Work?
A nationwide review of nearly 9,500 patient assessments submitted by 65 physicians practicing regenerative medicine in 43 clinics in 25 states revealed that:
- 73 percent of the patients treated with platelet rich plasma reported a meaningful reduction in pain within 12 months following treatment, especially those with tennis elbow (lateral epicondylitis) and knee osteoarthritis.
- 70 percent of the patients treated with adipose tissue therapy reported a meaningful reduction in pain within 12 months following treatment, with strong evidence shown by those treated for knee osteoarthritis.
- 61 percent of the patients treated with bone marrow aspirate reported a meaningful reduction in pain within 12 months following treatment, particularly those with knee osteoarthritis and low back pain.
This first-of-its-kind comprehensive review of patient-centered data reveals that for many patients, the regenerative power of orthobiologics provides new hope in treating orthopedic conditions without surgery. These outcomes, along with hundreds of published research on these treatments, provide evidence that the body’s own natural healing properties is a significant tool that physicians can use to provide orthopedic pain relief and to help their patients live a healthy, active live.
Drs. Christopher J. Rogers and Mary A. Ambach of San Diego Orthobiologics Medical Group together have successfully treated thousands of patients with PRP and cell-based treatments for more than three decades. Dr. Rogers is a co-author of “An Overview of Regenerative Treatments for Orthopedic Conditions: 2021 Outcomes Report” which aims to encourage innovative and effective regenerative treatments for orthopedic conditions.

Oct 23, 2020
Regenerative medicine represents a complete breakthrough in modern medicine. The body’s ability to heal itself naturally is actually not a new thing. A fractured bone will regrow and heal the break. Cut yourself shaving, and the skin will heal. There are many examples of our body’s innate ability to heal injuries.
Now modern science and technology are now enabling physicians to help their patients discover new ways in which the body can heal itself. Within the specialty of orthopedics, regenerative medicine is offering healing and pain relief to patients who suffer from conditions such as osteoarthritis, herniated discs or ligaments and tendons injuries.
Orthobiologics Can Boost the Body’s Own Natural Healing Abilities
Orthobiologics are cells and substances derived from cells that are naturally found in your body. By concentrating them and delivering them to the site of injury, they can help speed up the healing process.
Here’s how it works:
When you injure a bone, muscle or tendon, the platelet cells in the blood are the first responders arriving on the scene to quickly start healing. White blood cells also rush to the injury site to ward off infection, control inflammation and become the clean-up crew [i]. Other important cells like stem cells participate in this complex symphony of repair. Specialists in orthopedic regenerative medicine can now boost these natural processes through several specialized treatments that help maximize the body’s own innate healing capabilities.
Regenerative Treatments for Orthopedic Conditions
There are different orthobiologic treatments that your regenerative medicine specialist can recommend depending on your orthopedic condition:
· Platelet Rich Plasma puts the healing properties of the patient’s own blood to work to repair damaged joints, tendons and muscles. The platelets in the blood release growth factors and proteins that promote tissue repair, while the plasma carries the hormones, electrolytes and nutrients required to nourish cells during the healing process. PRP treatments are customized to the particular individual and their injury in order to be most effective.
· Cell based therapies use cells derived from the patient’s own bone marrow or adipose (fat) tissue. These cells include adult stem cells and many other healing cells. They produce molecules that direct neighboring cells in the area to form new blood vessels, decrease inflammation and encourage formation of new healthy tissues. Stem cells are special cells that have the unique ability to develop into the specific kind of cell needed, whether that be a tendon, ligament, cartilage or bone cell. Skilled regenerative medicine practitioners use highly specialized processes to prepare these cells that are then delivered directly to the injured area to stimulate healing.
· Prolotherapy (Proliferative Therapy) uses dextrose and other natural substances that are injected into a chronically injured ligament, tendon, nerves or joint in order to help the body jump-start its own natural healing response.
Beware of Imposters
As regenerative treatments have become more widely recognized for their ability to address orthopedic conditions and the chronic pain associated with it, more and more clinics are trying to get in on the action.
If you are considering regenerative treatments for pain related to osteoarthritis, tennis elbow, degenerative discs in the spine or other conditions, you should perform due diligence on the clinic that offers it. The source, processing and delivery of the regenerative materials are critical to the success of the treatment.
Currently, the U.S. Food and Drug Administration (FDA) does not allow the use of stem cells derived from birth tissue products (amniotic fluid and tissue, umbilical cord blood) to treat orthopedic conditions because these donor products have not been proven to be safe or effective. Our board-certified specialists only use your own cells (autologous) to treat orthopedic conditions.
Maximizing the effectiveness of these treatments requires a state-of-the-art facility and equipment, as well as knowledge and experience in fluoroscopic (x-ray) or ultrasound guidance to ensure targeted delivery of the healing cells to the injured area.
Orthobiologic treatments that capitalize on the body’s own natural healing abilities is one of the most exciting opportunities in modern medicine to address and resolve the chronic pain associated with orthopedic conditions that affects millions of Americans.
Drs. Christopher J. Rogers and Mary A. Ambach of San Diego Orthobiologics Medical Group together have successfully treated thousands of patients with cell based therapies for more than three decades. They are published authors and cell therapy researchers. Their facility in Carlsbad contains the most advanced Regenerative Medicine technology in San Diego and offers same day treatments with the highest level of safety and efficacy.
[i] https://www.aarp.org/health/alternative-medicine/info-11-2008/super_healing.html
[ii] https://orthoinfo.aaos.org/en/treatment/helping-fractures-heal-orthobiologics/
Jun 10, 2020
As one of the body’s largest joints, the hip gets its fair share of wear-and-tear over the years. The hip joint is a ball-and-socket joint, consisting of the femoral head at the top of the thighbone (ball) and the acetabulum in the pelvis bone (socket).
Chronic hip pain often develops in those over the age of 50, but can occur earlier, especially in those who are overweight or who have had a previous hip injury or surgery. Some people are born with abnormalities of the joint that put them at higher risk for hip issues as well.
Common symptoms of hip problems include:
- Groin pain
- Limping
- Decreased range of motion and stiffness
- Tenderness around the front or back of the hip
- Clicking, popping or locking of the joint
Why Do I Have Chronic Hip Pain?
Common causes of hip pain include:
- Osteoarthritis: chronic degeneration of the cartilage and inflammation of the hip tissues and joint fluid. The degeneration can be accelerated by trauma causing damage to the cartilage and subtle irregularities in how the hip developed in childhood.
- Bursitis: inflammation of the bursa, a fluid-filled sac that cushion the tendons overlying the bones
- Tendinitis and tendon tears: damage to the tendons in the hip, often from overuse or muscle weakness
- Labral tears: injury to the labrum, a soft cartilage tissue that surrounds the hip socket
- Sacroiliitis: Inflammation of the sacroiliac joints where your lower spine and pelvis connect.
- Avascular necrosis: impaired blood flow to the hip bone causes damage
The good news for patients suffering from chronic hip pain is that advances in regenerative medicine are giving hope to those who feared that total joint replacement therapy was their only option.
San Diego Orthobiologics Medical Group offers several advanced regenerative therapies for hip joint pain:
- Platelet Rich Plasma Therapy uses growth factors from the platelets in the patient’s own blood by releasing substances called growth factors concentrates platelets to stimulate tissue healing for degenerative joints and soft tissue injuries.
- ENDORET PRGF (platelet rich in growth factors) contains proteins that stimulate the tissue repair processes, including new blood vessel formation, cell mobilization and cell proliferation. PRGF can accelerate healing and minimize inflammation that reduces pain.
- Bone Marrow Aspirate Concentrate (BMAC): utilizes your own bone marrow which contains cells that have the ability to improve circulation, decrease inflammation and promote healing in tendons, ligaments and cartilage. BMAC provides highly concentrated regenerative cells to support a robust healing response through a simple office procedure.
- LIPOGEMS® is an FDA-compliant device for processing and same-day use of your own adipose tissue (fat) to treat joint and tendon injuries. Adipose tissue is a rich source of adipose derived stem cells and other regenerative orthobiologics.
- Prolotherapy, also known as “proliferative therapy,” delivers dextrose and other medications to help regenerate tissue and stimulate a healing response in a chronically injured ligament, tendon or joint. Prolotherapy is often combined with PRP therapy to expedite healing.
- Alpha 2 Microglobulin (A2M) uses uses orthobiologics from a patient’s own blood to stop the progression of joint degeneration, decrease inflammation and promote tissue healing.
These treatments offer better safety than most surgical procedures as they are minimally invasive and are performed in our office procedure suite. Patients do not require hospitalization, or a lengthy recovery. Many patients are able to resume normal activities within days of their treatment and see pain relief within weeks.
Drs. Christopher Rogers and Mary Ambach of San Diego Orthobiologics Medical Group are leaders in the field of regenerative medicine for orthopedic conditions. They were the first in San Diego to use Lipogems® as well as ENDORET PRGF therapy for the treatment of orthopedic conditions.
Sources:
https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/
https://www.mayoclinic.org/diseases-conditions/sacroiliitis/symptoms-causes/syc-20350747
https://www.mayoclinic.org/symptoms/hip-pain/basics/causes/sym-20050684

May 1, 2020
Orthobiologics research has come a long way since the earliest reports of platelet rich plasma (PRP) in the 1980s and stem cells in the 1960s. There has been exponential growth in the number of published scientific studies on PRP and stem cells in orthopedics over the past 10 years.
Regenerative medicine is a new medical specialty that uses advancements in the study of cells and tissue engineering to understand how the body heals itself. In the field of orthopedics, regenerative treatments have evolved to capitalize on the unique healing qualities of our own cells to stimulate healing, reduce inflammation and decrease pain for a variety of musculoskeletal conditions.
The demand for regenerative treatments continues to grow as patients discover how these treatments are successfully being used to treat acute musculoskeletal injuries and degenerative conditions. More and more patients have benefited from such therapies with reduction in pain and significant improvement in their quality of life.
Regenerative Medicine in 2020
Clinical trials and research in regenerative medicine has provided more ever increasing evidence for the safety and efficacy of cell based therapies when used in orthopedics such as osteoarthritis, tendon tears, ligament injuries, low back pain, sciatica and several others conditions.
The choice of regenerative treatment depends upon multiple factors including the type and severity of injury, medical comorbidities and other issues unique to each patient. San Diego Orthobiologics Medical Group offers a number of regenerative medicine options such as:
- Platelet Rich Plasma Therapy: Growth factors and proteins in the platelets and plasma of the patient’s own blood promote tissue repair and reduce inflammation. Specific PRP formulation is customized to joints, tendons, ligament or nerves for maximum results.
- Adipose Derived Stem Cell Therapy: Fat tissue derived from your own body enables regenerative cells (such as stem cells) within your own fat tissue to work together and repair, reconstruct and replace damaged or injured tissues.
- Bone Marrow Aspiration Concentrate (BMAC): Utilizes regenerative cells that are contained within your own bone marrow. The marrow contains a rich reservoir of anti-inflammatory molecules, platelets and stem cells to stimulate your body’s ability to improve circulation, decrease inflammation and regenerate tissues.
- Prolotherapy: Medications that help regenerate tissue and relieve pain are injected into injured ligaments, tendons or joints to strengthen and improve stability in patients with osteoarthritis, ligament sprains and sports-related injuries.
Moving Forward
The field of regenerative medicine is continuously evolving and expanding. Cell based therapies are getting acknowledgement in orthopedic surgery and have been used to accelerate healing and improve outcomes. The combined use of cells and protein scaffolds (tissue framework) are utilized for cartilage, tendon, ligament and bone tissue engineering to accelerate healing and long lasting results. Surgery to repair bone fractures or bone defects have been supplemented with cell therapy to increase bone healing and mineralization.
Many other exciting potential applications for stem cell therapy are currently being studied, not just in orthopedics, but in other specialties. The idea that a patient can bank their own stem cells to store for future use is already a reality.
However, there is still more work to be done in order to make significant progress on this field. Although there are thousands of studies published in peer-reviewed scientific journals, there is a great need for more high-quality studies and clinical trials. Continued work on standardization of processes, reporting and treatment protocols is vital. Collection of data through registries is not only important to track patient complications and outcomes, but also to guide future decisions made by insurance companies and regulators. Collaboration with a multidisciplinary team of experts in physical medicine and rehabilitation, orthopedic surgery, sports medicine, cell therapy, molecular biology and others will continue to move the field forward at a rapid pace.
Drs. Christopher J. Rogers and Mary A. Ambach of San Diego Orthobiologics Medical Group are experts and leaders in the field of regenerative medicine. They are involved in clinical trials using cell-based therapies for knee osteoarthritis and disc degeneration in the lumbar spine. They have published in multiple medical journals and Regenerative Medicine textbooks. They serve as faculty members and lecturers at national and international medical conferences and serve on the board of directors for several regenerative medicine organizations.