Jan 15, 2025
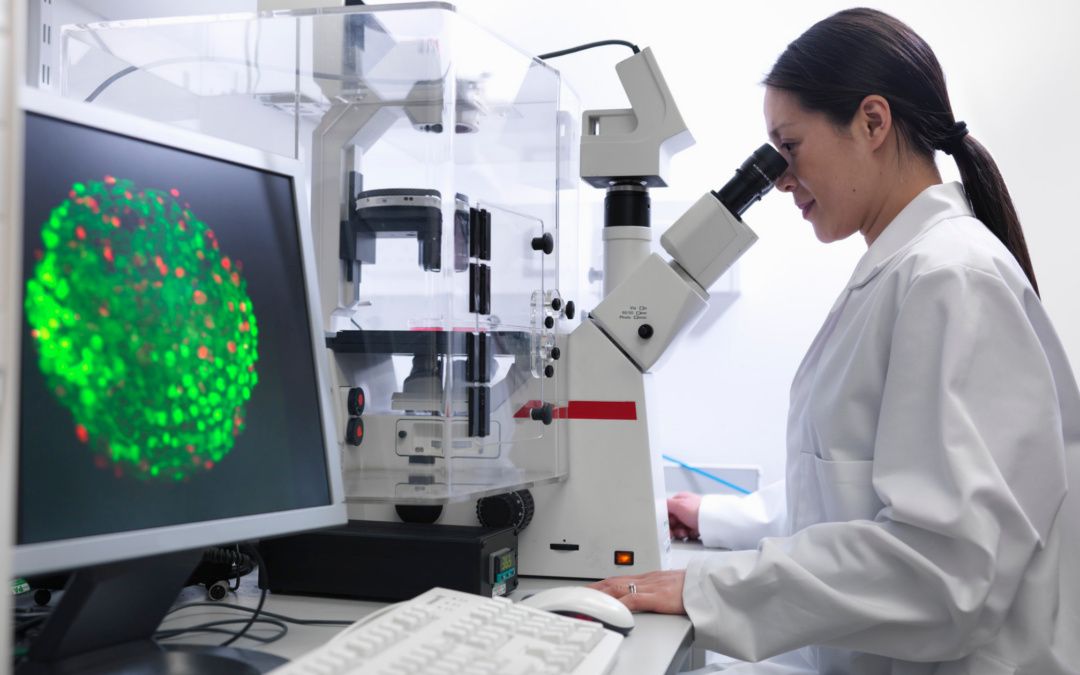
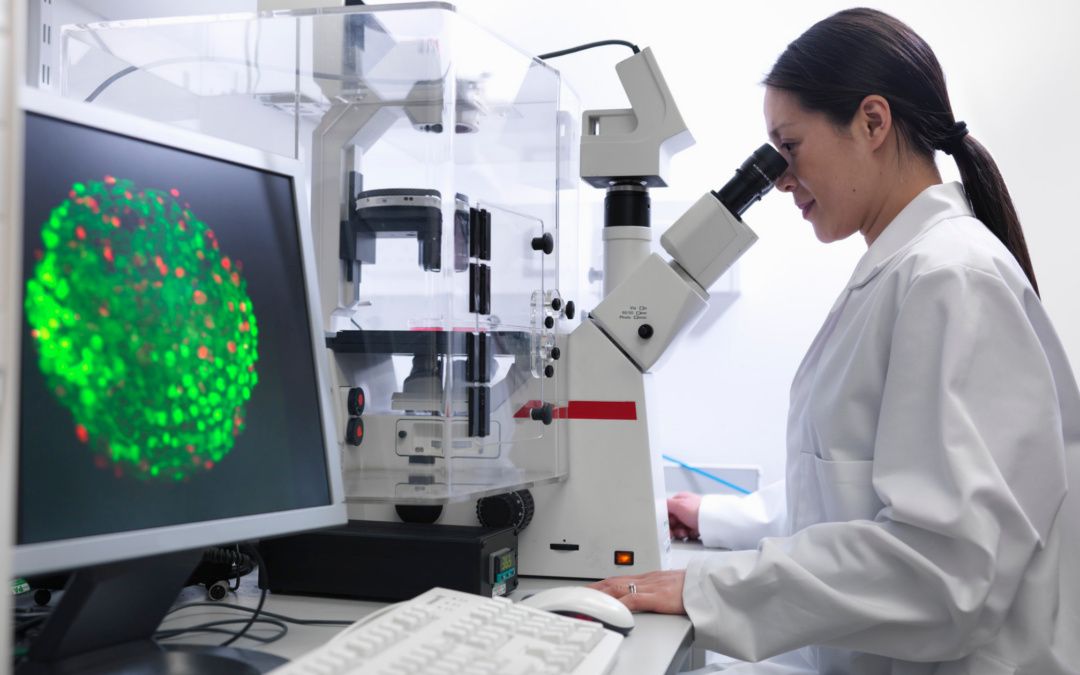
As researchers and medical professionals delve deeper into the world of cellular therapy, understanding its efficacy has become a crucial area of focus. Efficacy, in this context, refers to the ability of a particular treatment or intervention to produce the desired therapeutic effect under controlled conditions. By examining the efficacy of cellular therapy, healthcare providers can make informed decisions about the most appropriate and effective treatment options for their patients, ultimately leading to better overall patient care and outcomes.
Understanding the Efficacy of Cellular Therapy
The efficacy of cellular therapy is a multifaceted concept, influenced by a variety of factors. To fully comprehend the effectiveness of this approach, it is essential to explore the various aspects that contribute to its success.
One of the key factors in determining the efficacy of cellular therapy is the specific type of cells being used. Different cell types, such as stem cells, immune cells, or tissue-specific progenitor cells, have unique properties and capabilities that can impact their therapeutic potential. The source of these cells, whether they are derived from the patient’s own body (autologous) or from a donor (allogeneic), can also play a significant role in the therapy’s efficacy.
Another crucial aspect is the method of cell delivery. Cellular therapies can be administered through various routes, such as intravenous infusion, direct injection into the target tissue, or even implantation of engineered tissue constructs. The choice of delivery method can significantly influence the cells’ ability to reach and integrate with the damaged or diseased area, ultimately affecting the overall efficacy of the treatment.
Furthermore, the specific medical condition being treated is a key determinant of cellular therapy’s efficacy. Different diseases and injuries may respond differently to the same cellular therapy, as the underlying pathophysiology and the cellular and molecular mechanisms involved can vary greatly. Consequently, the efficacy of cellular therapy may be more pronounced in certain disease states compared to others.
Factors Affecting the Efficacy of Cellular Therapy
The efficacy of cellular therapy is influenced by a complex interplay of various factors, both intrinsic and extrinsic to the therapy itself. Understanding these factors is crucial in optimizing the effectiveness of this innovative approach to healthcare.
Intrinsic Factors
- Cell Type and Source: As mentioned earlier, the specific type of cells used in the therapy, as well as their source (autologous or allogeneic), can significantly impact the efficacy of the treatment.
- Cell Potency and Function: The inherent potency and functional capabilities of the cells used in the therapy are critical determinants of their ability to effectively repair, regenerate, or modulate the target tissue or disease.
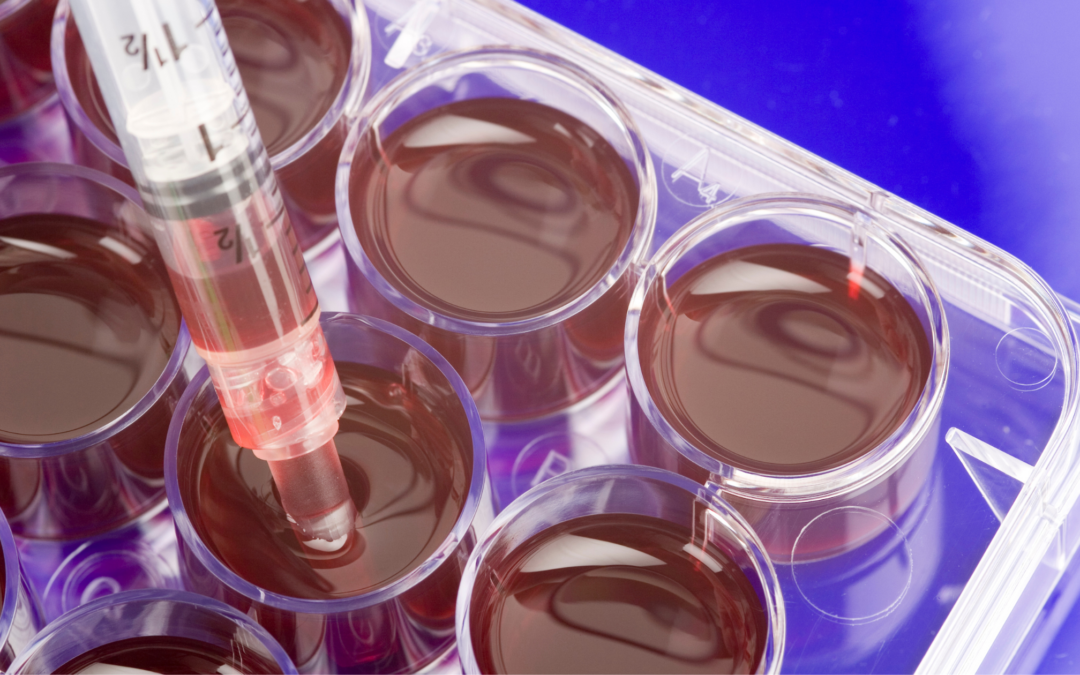
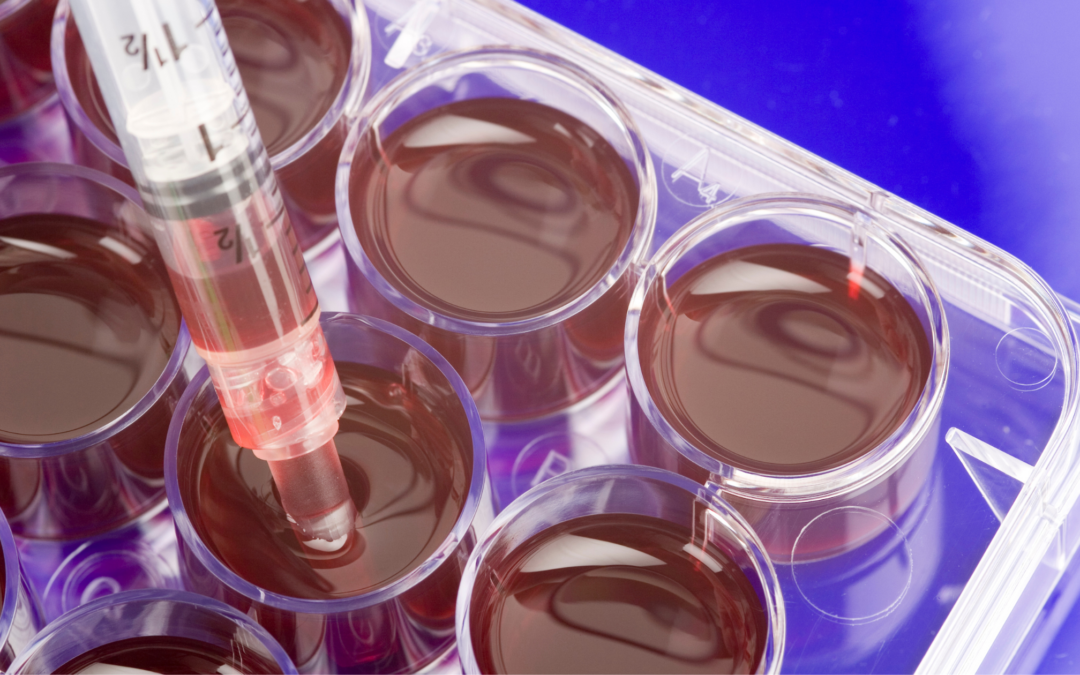
- Cell Viability and Purity: Maintaining the viability and purity of the cells throughout the manufacturing and delivery process is essential to ensure their optimal therapeutic potential.
- Cell Expansion and Manipulation: The methods used to expand and manipulate the cells, such as in vitro culture conditions and genetic engineering, can influence their therapeutic properties and efficacy.
Extrinsic Factors
- Delivery Route and Timing: The method and timing of cell delivery can greatly impact the cells’ ability to reach and engraft within the target tissue, thereby affecting the overall efficacy of the therapy.
- Microenvironmental Factors: The specific characteristics of the target tissue or disease environment, such as inflammation, hypoxia, or the presence of inhibitory factors, can influence the cells’ ability to survive, proliferate, and exert their intended therapeutic effects.
- Patient-Specific Factors: Individual patient characteristics, such as age, underlying health conditions, and immune status, can play a significant role in the efficacy of cellular therapy.
- Regulatory and Manufacturing Considerations: The regulatory framework and manufacturing processes involved in the development and production of cellular therapies can impact their quality, consistency, and ultimately, their efficacy.
Future Advancements and Potential of Cellular Therapy
As the field of cellular therapy continues to evolve, researchers and healthcare professionals are actively exploring new frontiers to further enhance the efficacy and potential of this innovative approach. Several exciting advancements and areas of exploration are shaping the future of cellular therapy:
- Stem Cell Technology: Ongoing research into the use of different types of stem cells, such as embryonic, induced pluripotent, and adult stem cells, is aimed at unlocking their full therapeutic potential and improving their efficacy in a wide range of medical applications.
- Genetic Engineering and Cell Modification: Advances in genetic engineering and cell manipulation techniques are enabling the development of genetically modified or engineered cells with enhanced therapeutic properties, potentially leading to improved efficacy and targeted treatments.
- Combination Therapies: The integration of cellular therapy with other treatment modalities, such as biomaterials, drugs, or even other cell-based approaches, is being explored to create synergistic effects and improve overall efficacy.
- Personalized Medicine: The growing emphasis on personalized and precision medicine is driving the development of tailored cellular therapies that are optimized for individual patient needs, taking into account their unique genetic, molecular, and clinical profiles.
- Improved Delivery and Targeting: Researchers are investigating innovative methods of cell delivery and targeting, such as the use of biomimetic materials, nanoparticles, or tissue-specific homing strategies, to enhance the cells’ ability to reach and integrate with the target tissue.
- Real-World Evidence and Data Analytics: The collection and analysis of real-world data on the use and outcomes of cellular therapies will provide valuable insights into their efficacy, safety, and long-term effects, ultimately informing clinical decision-making and driving further advancements.
The Promising Future of Cellular Therapy and Its Efficacy in Improving Patient Outcomes
As the field of cellular therapy continues to evolve, the promise of this innovative approach to healthcare becomes increasingly evident. By harnessing the inherent regenerative and therapeutic capabilities of living cells, cellular therapies hold the potential to revolutionize the way we treat a wide range of medical conditions, from chronic diseases to acute injuries.
The ongoing research and development in this field are steadily uncovering new ways to enhance the efficacy of cellular therapies. From advancements in stem cell technology and genetic engineering to the integration of personalized medicine and improved delivery methods, the future of cellular therapy looks increasingly bright.
As healthcare providers and researchers work together to better understand the factors that influence the efficacy of cellular therapies, they can make more informed decisions about the most appropriate and effective treatment options for their patients. This, in turn, can lead to improved patient outcomes, reduced reliance on traditional, more invasive treatments, and a greater overall quality of life for those who benefit from these innovative therapies.
To learn more about the latest advancements in cellular therapy and how it can benefit your healthcare needs, schedule a consultation with one of the experts at San Diego Orthobiologics Medical Group today. Our team is dedicated to providing personalized, evidence-based solutions to help you achieve your optimal health and wellness.

Aug 14, 2023
Hand and wrist injuries can occur to an individual either suddenly, such as in the case of a sprain, or over time, such as through repetitive use injuries. In either case, the sufferer needs to know about the pain relief options that are available to them. Given the myriad of different ways that one can injure their hand and/or wrist, it is challenging to diagnose a patient without a full medical evaluation. The good news is that cell therapies provide a bright future in pain relief for individuals suffering from hand and wrist pain of most varieties.
What is Cell Therapy?
The use of cell therapy is rapidly expanding as many more people become informed of the option and become more familiar with it. Dr. Rogers of the San Diego Orthobiologics Medical Group offers the following explanation of what cell therapy is and why it matters:
Cell-based therapies are a versatile and powerful treatment method that is transforming orthopedic medicine. Conditions such as arthritis, tendon tears or disc tears traditionally managed with medications or surgery can now be treated with your own cells to provide years of relief.
The natural healing benefits that many patients experience are significant and point to the idea that cell therapy should be a first-choice option for many patients. If they can use their own body’s cells to work on healing themselves, why not give this a try.
The Types of Cell Therapy You May Be Offered
Different types of cell therapies might be useful when working on finding relief from hand and wrist pain. For example:
- Platelet-Rich Plasma (PRP) Injections – Platelets from the patient’s own blood are concentrated and then injected to area of damaged tissue to stimulate healing. These platelets release growth factors and proteins that promote tissue regeneration.
- Adipose (fat) tissue injections or Bone marrow injections – Cells are harvested from patient’s fat tissue or pelvic bone. These cells spur the production of new blood vessels, awaken stem cells and encourage newly forming cells to produce collagen and other proteins essential for creating new healthy tissues. These specific cells can stimulate tissue regeneration.
Minimal Invasiveness and Recovery Time
When looking for medical interventions for pain relief, most patients are concerned with two primary things. First, they want to ensure that the procedure they receive will be as minimally invasive as possible. Secondly, they want something that doesn’t involve a long recovery period if they can avoid it. After all, we all have busy lives and can’t afford to miss out on too much of it. The good news is that cell therapy is minimally invasive and involves only a short recovery period.
Reduced Pain, Improved Mobility
The two biggest things that those suffering from hand and wrist pain want from any treatment that they receive are improved mobility and reduced pain. Those who opt to undergo cell therapy will receive both. These therapies provide cells to areas within the body that are degenerated and need care. Doing so offers faster recovery periods and results in far fewer complications than other treatment options such as surgery. All of this is critically important when it comes to receiving the care and support that you require.
You can receive the care you require and get back to living the life that you want to live. Don’t hesitate to contact us and learn more about the cell therapy you can receive to get past the pain you are suffering from now.

Oct 13, 2022
As one the largest joints in the body, the knees often suffer the most from the wear-and-tear that comes with a lifetime of use (or abuse). Whether damaged by an injury such as a ligament or tendon tear, or simply worn down by years of standing, running, jumping, lifting, etc., the result is often the same: chronic pain, inflammation, and reduced movement.
Depending on the extent of the injury or damage to the knee, patients can often gain some temporary relief from steroid injections that decrease swelling or from other interventional treatments such as hyaluronic acid injections that increase lubrication in the joint. But when these options have been expended, many look to surgery as their last, best hope to repair the damage and bring sought-after pain relief.
But now, non-surgical cellular treatments are providing long-term relief to patients with knee pain by putting the body’s own natural healing abilities to work to undo the damage brought on by injury or degeneration.
How Do Cellular Treatments Work?
Known as regenerative medicine, cellular treatments harness powerful healing properties within the body’s building blocks—its own cells—to help repair and, in some cases, replace injured tissues. These treatments promote healing of injuries to the cartilage in the knee joint, as well as soft tissues such as tendons and ligaments in the knee.
To adhere to Federal Food and Drug Administration (FDA) guidelines, only autologous (from the patient’s own body) cellular products can be used to treat orthopedic conditions. Donor products, including cord or amniotic cells, are not approved to treat knee osteoarthritis or soft tissue injuries in the knee.
Cellular products are taken from the patient’s own blood, bone marrow, or fat (adipose) tissues to maximize the benefits of their unique healing properties:
- Platelet Rich Plasma: Platelets in blood release growth factors and proteins that promote tissue repair, while the plasma carries the hormones, electrolytes and nutrients required to nourish cells during the healing process. Platelet rich plasma treatments can be customized to create specific formulations for each type of tissue being treated (muscle, tendon, ligament, cartilage).
- Cellular Therapy: Cells derived from the patient’s own bone marrow or adipose (fat) tissue called “pericytes” produce molecules that spur the production of new blood vessels, awaken other stem cells and encourage newly forming cells to produce collagen and other proteins essential for creating new healthy tissues. These specific cells can develop into the specific kind of cell needed, whether that be tendon, ligament, cartilage, or bone.
After these products are removed from the patient, they are concentrated and reinjected directly to the injured area to address the degeneration or injury.
Do Cellular Treatments for the Knees Work?
Regenerative medicine practitioners have scores of anecdotal evidence from satisfied patients that support the powerful pain-relieving and healing properties of cellular treatments for the knees.
But because the field of regenerative medicine is relatively new, until recently, there has been a limited amount of clinical data to bolster this anecdotal evidence. We believe the quantitative, controlled data that clinical trials will produce will not only further the use of cellular treatments for orthopedic conditions but will also confirm what hundreds of our satisfied patients have been telling us for years: cellular treatments have helped their bodies heal naturally while allowing them to resume the activities that help them regain their quality of life.
The experts at SDOMG help patients with knee injuries and knee osteoarthritis find the relief they need using expert technology and treatments. To learn more about cellular therapy for knee injuries, contact SDOMG using the form below.
May 27, 2022
Orthobiologics is a combination of words: “ortho” refers to the body’s musculoskeletal system (muscles, bones, joints, ligaments, and tendons), and “biologics” refers to naturally derived substances used to heal parts of the body. Orthobiologic treatments can be used to harness the body’s ability to heal itself to restore or establish normal function. Within the field of orthopedics, these specific treatments hold great promise for helping patients with injuries or degeneration in the musculoskeletal system.
When joints, ligaments, tendons, or discs are damaged, it can lead to chronic pain in the:
- Lower Back
- Knees
- Hips
- Neck
- Feet and ankles
- Hands and wrists
- Elbows and Shoulders
Orthobiologics promote healing and stimulate growth of new healthy tissues. When the underlying cause is treated, pain improves or resolves.
How Do Orthobiologics Work?
Orthobiologic treatments for orthopedic conditions use the patient’s own blood and cells (known as autologous products) to kick-start the body’s own healing processes. These biologic products are collected from the patient and concentrated to isolate the healing proteins, molecules, and nutrients they contain. These super-healers are then re-injected into the exact site of the damaged tissue to encourage new cell growth and healing.
Limitations on Cellular Treatments by the FDA
The U.S. Food & Drug Administration (FDA) does not allow the use of embryonic or blood cord products for treating orthopedic conditions. The FDA also banned certain language and vague advertising regarding these types of products that in the past have opened doors to illegal markets cell-buying and procedures that are potentially dangerous to patients.
Skilled certified physicians can use the following autologous (from your own body) cellular products to treat musculoskeletal problems, provided they follow the FDA’s guidelines for safety and efficacy:
- Platelet Rich Plasma: Platelets in the patient’s own blood release growth factors and proteins that promote tissue repair, while the plasma carries cytokines and nutrients required to nourish cells during the healing process.
- Cellular Therapies: A specific type of cells, called mesenchymal cells, taken from the patient’s own fat tissue (adipose) or bone marrow, have the unique ability to develop into the specific kind of cell needed to promote healing and possess molecules that direct other cells in the injured area to form new blood vessels, awaken other cells, and encourage newly forming cells to produce collagen and other proteins essential for creating new healthy tissues.
Because the platelet-rich plasma and mesenchymal cells are taken directly from the patient and delivered back to them, they do not present the risk of allergic reactions or some infections seen with donor products.
Are PRP and Cell Therapies Painful?
For many years, patients with unresolved chronic orthopedic pain were left to consider surgery as their best hope for long-term pain relief. But with advancements in regenerative medicine, some patients can avoid major surgery and lengthy rehab.
Orthobiologic treatments are conducted with needles. Blood plasma and mesenchymal cells are aspirated (removed via a needle) and reinjected through a needle. There are no large incisions, which means the risk of bleeding and infection is significantly reduced. It also means that the procedures can be performed on an outpatient basis, and recovery begins at home within hours of the treatment.
Best of all, patients can enjoy long-lasting pain relief and enjoy an improved quality of life without chronic pain.
Ask the Right Questions, Get the Best Results
When considering regenerative medicine to treat orthopedic conditions, patients should make sure:
- The physician performing the procedure is board-certified
- Advanced centrifuge technology is used to prepare the cellular products so that they offer the highest possible concentrations of healing properties.
- Treatments are given under fluoroscopic (X-ray) or ultrasound guidance to ensure precise delivery of the regenerative products to the exact site of the injury.
- The practice acknowledges and strictly follows FDA guidelines for the use of cellular products to treat musculoskeletal damage.
The best outcomes occur when the patient understands the benefits of regenerative treatments and knows the right questions to ask prior to the procedure.
SDOMG is a state-of-the-art practice focusing on Orthobiologics to treat orthopedic conditions. To learn more about the procedures they provide, visit their website or fill out the form below. We look forward to helping you regain your quality of life.
Nov 26, 2021
Medical research advances enable physicians to find new and innovative ways to use the body’s systems to fight disease and injury.
Regenerative medicine is a field of medicine that uses the body’s own cells and tissues to heal injuries and medical conditions. In the treatment of cancer the cells are used in immunotherapy, which involves modifying patient’s cells to fight the disease. In the field of orthopedics, regenerative medicine specialists use the patient’s own blood cells, bone marrow or adipose tissue to help the body boost its own natural healing properties. These are known as orthobiologics.
At the present time, FDA allows the use of autologous orthobiologics —which means the tissue or cells used must come from the same patient. Donor products are not allowed to be used in clinical setting unless it is used under the purview of a clinical trial. Read here on the FDA guidance on the use of human cells and tissues.
Cell-based Treatments for Orthopedic Conditions
There are two types of cell-based therapies that can be used to treat orthopedic conditions:
Bone Marrow Aspiration Concentrate (BMAC): Bone marrow-derived cells are collected from the back of the pelvic bone. The marrow contains mesenchymal stem cells which have the ability to renew themselves and differentiate into bone, tendon, cartilage and muscle cells. These make them an ideal therapy for treating orthopedic injuries such as tendon tears, worn cartilage, and degenerated disc disease. BMAC also contains important therapeutic cells, growth factors and proteins that stimulate the body’s natural ability to improve circulation, decrease inflammation and heal injured tissues.
Micro-fragmented Adipose Tissue (fat) Cells: Adipose-derived cells are collected from a fat sample usually from the buttock or abdomen. There is minimal manipulation of the tissue with no enzymatic digestion or addition of other biological or pharmacological agents. Fat or adipose tissue is rich in healing cells like mesenchymal stem cells or MSCs, growth factors and other proteins that can assist in healing tissues.
Why Consider Cell-Based Therapies?
There is increasing body of clinical research that demonstrates the safety and efficacy of Cell based therapies. A recent comprehensive report 1 based on actual clinical data collected from 65 physicians at 43 clinics in 25 states revealed that seventy percent of the patients treated with adipose tissue therapy reported a meaningful reduction in pain at 12 months following treatment and sixty-one percent of the patients treated with bone marrow aspirate reported a meaningful reduction in pain at12 months following treatment.
Micro-fragmented adipose tissue or bone marrow aspirate concentrate is a non-surgical treatment option that does not involve incisions, general anesthesia, hospitalizations or lengthy rehabilitation stays. This is an outpatient procedure performed in a doctor’s clinic using only local anesthesia.
Patients considering cell-based therapies should do their research in ensuring they get the best treatment. There are several important factors that can impact the effectiveness of these treatments. These include:
- Cellular product preparation: The patient’s bone marrow or fat tissue must be processed using FDA compliant devices and protocols. It must be prepared in a safe and sterile environment by medical personnel who are trained in the proper handling of these tissues.
- Delivery: The procedure must be performed by skilled physicians who are properly trained in this field. They must be able to perform these highly specialized injection techniques using imaging guidance to ensure that the cellular products are delivered to the site of injury.
- Experience: The field of regenerative medicine is changing daily and there are a limited number of specialists around the country who have the experience and technology to perform cell-based orthopedic treatments safely and effectively. Dr. Mary A. Ambach and Dr. Chris Rogers have decades of experience in using regenerative therapies and are nationally recognized experts in this field.
1Databiologics. An Overview of Regenerative Treatments for Orthopedic Conditions. 2021 Outcomes Report.