May 27, 2022
Orthobiologics is a combination of words: “ortho” refers to the body’s musculoskeletal system (muscles, bones, joints, ligaments, and tendons), and “biologics” refers to naturally derived substances used to heal parts of the body. Orthobiologic treatments can be used to harness the body’s ability to heal itself to restore or establish normal function. Within the field of orthopedics, these specific treatments hold great promise for helping patients with injuries or degeneration in the musculoskeletal system.
When joints, ligaments, tendons, or discs are damaged, it can lead to chronic pain in the:
- Lower Back
- Knees
- Hips
- Neck
- Feet and ankles
- Hands and wrists
- Elbows and Shoulders
Orthobiologics promote healing and stimulate growth of new healthy tissues. When the underlying cause is treated, pain improves or resolves.
How Do Orthobiologics Work?
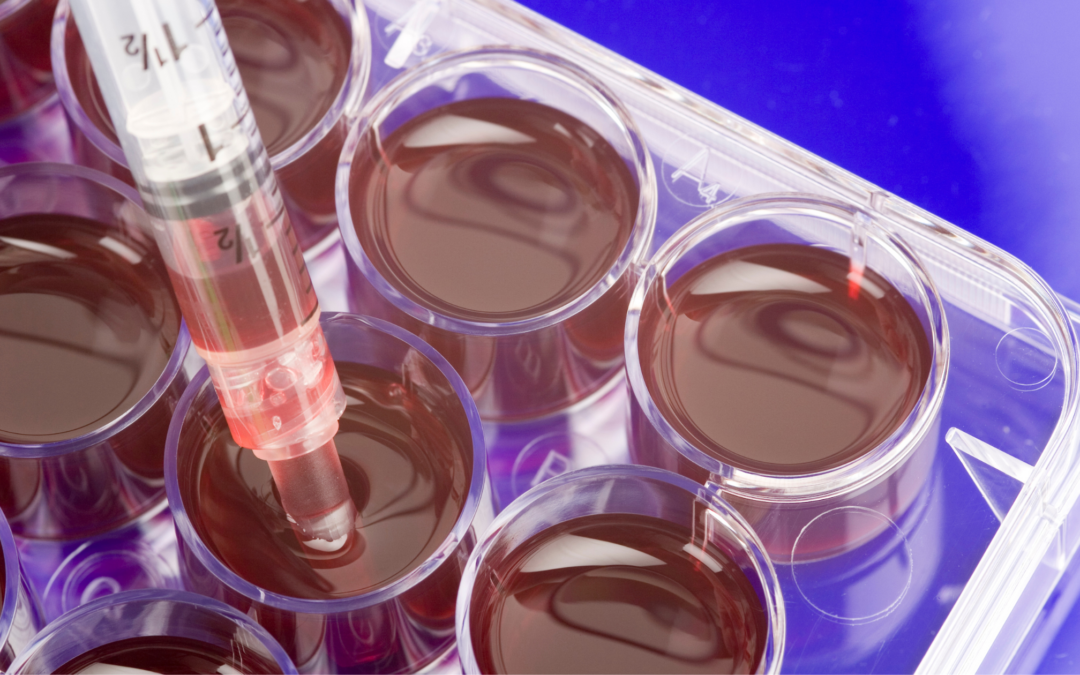
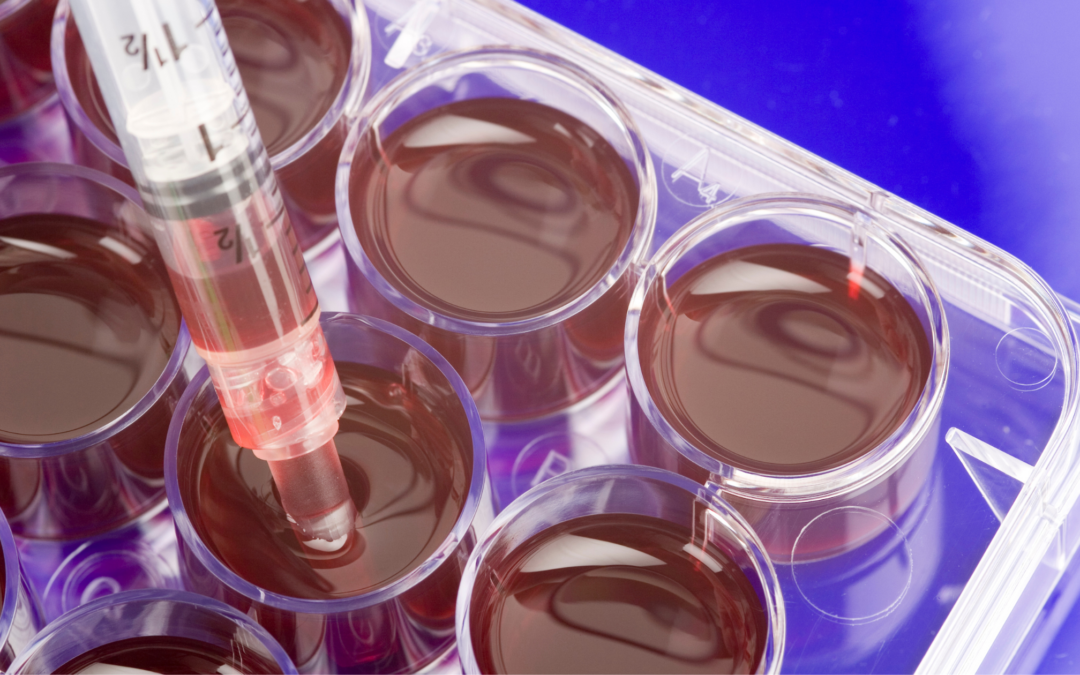
Orthobiologic treatments for orthopedic conditions use the patient’s own blood and cells (known as autologous products) to kick-start the body’s own healing processes. These biologic products are collected from the patient and concentrated to isolate the healing proteins, molecules, and nutrients they contain. These super-healers are then re-injected into the exact site of the damaged tissue to encourage new cell growth and healing.
Limitations on Cellular Treatments by the FDA
The U.S. Food & Drug Administration (FDA) does not allow the use of embryonic or blood cord products for treating orthopedic conditions. The FDA also banned certain language and vague advertising regarding these types of products that in the past have opened doors to illegal markets cell-buying and procedures that are potentially dangerous to patients.
Skilled certified physicians can use the following autologous (from your own body) cellular products to treat musculoskeletal problems, provided they follow the FDA’s guidelines for safety and efficacy:
- Platelet Rich Plasma: Platelets in the patient’s own blood release growth factors and proteins that promote tissue repair, while the plasma carries cytokines and nutrients required to nourish cells during the healing process.
- Cellular Therapies: A specific type of cells, called mesenchymal cells, taken from the patient’s own fat tissue (adipose) or bone marrow, have the unique ability to develop into the specific kind of cell needed to promote healing and possess molecules that direct other cells in the injured area to form new blood vessels, awaken other cells, and encourage newly forming cells to produce collagen and other proteins essential for creating new healthy tissues.
Because the platelet-rich plasma and mesenchymal cells are taken directly from the patient and delivered back to them, they do not present the risk of allergic reactions or some infections seen with donor products.
Are PRP and Cell Therapies Painful?
For many years, patients with unresolved chronic orthopedic pain were left to consider surgery as their best hope for long-term pain relief. But with advancements in regenerative medicine, some patients can avoid major surgery and lengthy rehab.
Orthobiologic treatments are conducted with needles. Blood plasma and mesenchymal cells are aspirated (removed via a needle) and reinjected through a needle. There are no large incisions, which means the risk of bleeding and infection is significantly reduced. It also means that the procedures can be performed on an outpatient basis, and recovery begins at home within hours of the treatment.
Best of all, patients can enjoy long-lasting pain relief and enjoy an improved quality of life without chronic pain.
Ask the Right Questions, Get the Best Results
When considering regenerative medicine to treat orthopedic conditions, patients should make sure:
- The physician performing the procedure is board-certified
- Advanced centrifuge technology is used to prepare the cellular products so that they offer the highest possible concentrations of healing properties.
- Treatments are given under fluoroscopic (X-ray) or ultrasound guidance to ensure precise delivery of the regenerative products to the exact site of the injury.
- The practice acknowledges and strictly follows FDA guidelines for the use of cellular products to treat musculoskeletal damage.
The best outcomes occur when the patient understands the benefits of regenerative treatments and knows the right questions to ask prior to the procedure.
SDOMG is a state-of-the-art practice focusing on Orthobiologics to treat orthopedic conditions. To learn more about the procedures they provide, visit their website or fill out the form below. We look forward to helping you regain your quality of life.

Feb 6, 2022
Whether due to degenerative arthritis or injury, the Agency for Healthcare Research and Quality reports that more than 450,000 total hip replacements are performed in the United States every year.[i]
Even though this is major surgery and requires hospitalization and lengthy rehab, many patients who suffer from chronic hip pain believe they have no other options.
Thanks to the advances in the field of regenerative medicine, they do.
Why Do My Hips Hurt?
Hip degeneration or tissue damage can result in pain, tenderness, “clicking” and reduced range of motion. Pain can be localized in the front, side, or back of the hip.
Hip pain can have many causes, including:
- Degenerative osteoarthritis. Occurs when the cartilage between the bones of the hip joint begins to break down, usually with age.
- Tendon tears and tendinosis. Overuse may result in a tear or degeneration of the tendons, the thick bands of tissue that attach the hip bones to neighboring muscles.
- Muscle or tendon strains. Often the result of repetitive motions that stretch the muscles, tendons, and ligaments that support the hips.
- Hip labral tear. The labrum is a ring of cartilage that covers the outside rim of the hip socket. It cushions the joint and helps hold the femur (thighbone) ball within your hip socket. Anyone who makes repetitive twisting movements of the hip joint can develop labral tears.
- Obesity. Carrying extra weight puts tremendous pressure on the hips and can significantly hasten joint degeneration.
- In some cases, congenital abnormalities may also cause hip pain, as can previous surgery or trauma.
Using the Body’s Natural Healing Abilities to Treat Hip Pain
For those suffering from chronic hip pain, regenerative biologic therapies are providing new hope for pain relief without major surgery.
Regenerative medicine specialists use the natural healing properties in the patient’s own cells to stimulate healing of damaged tissues, reduce inflammation, and in some cases, promote the growth of new cells.
There are two types of regenerative biologic therapies used in clinical practice to treat orthopedic conditions, including hip pain.
- Platelet Rich Plasma (PRP): A concentrated solution of platelets derived from the patient’s own blood which contains a significant amount of growth factors and proteins that promote tissue regeneration, decrease inflammation, and encourage blood vessel formation.
- Cell-Based Therapies: Cells taken from the patient’s own fat tissue (Microfragmented Adipose Tissue) or bone marrow (Bone Marrow Aspiration Concentrate) which contain adult stem cells that have the unique ability to renew themselves and develop into other cell types which promote tissue healing. These cells control pain, decrease inflammation, and fight infection.
How are these Biologic Therapies Performed?
Biologic therapies are injection procedures. Blood, bone marrow, or fat tissue is collected and processed, and then injected into the injured tissue on the same day. These procedures are performed on an out-patient basis and recovery begins at home within hours of the treatment. There are no large incisions, no lengthy hospitalizations, or rehab stays involved.
Most hip tendon injuries and osteoarthritis respond well to these orthobiologic treatments. Factors such as the degree of injury or degeneration, as well as the patient’s overall health, can impact the final outcomes, but for patients weighing invasive surgery, orthobiologics can provide an option for pain relief and healing without surgery.
To learn more about healing hip pain with biologic therapies, fill out the form below to learn more:
[i] https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/
Nov 26, 2021
Medical research advances enable physicians to find new and innovative ways to use the body’s systems to fight disease and injury.
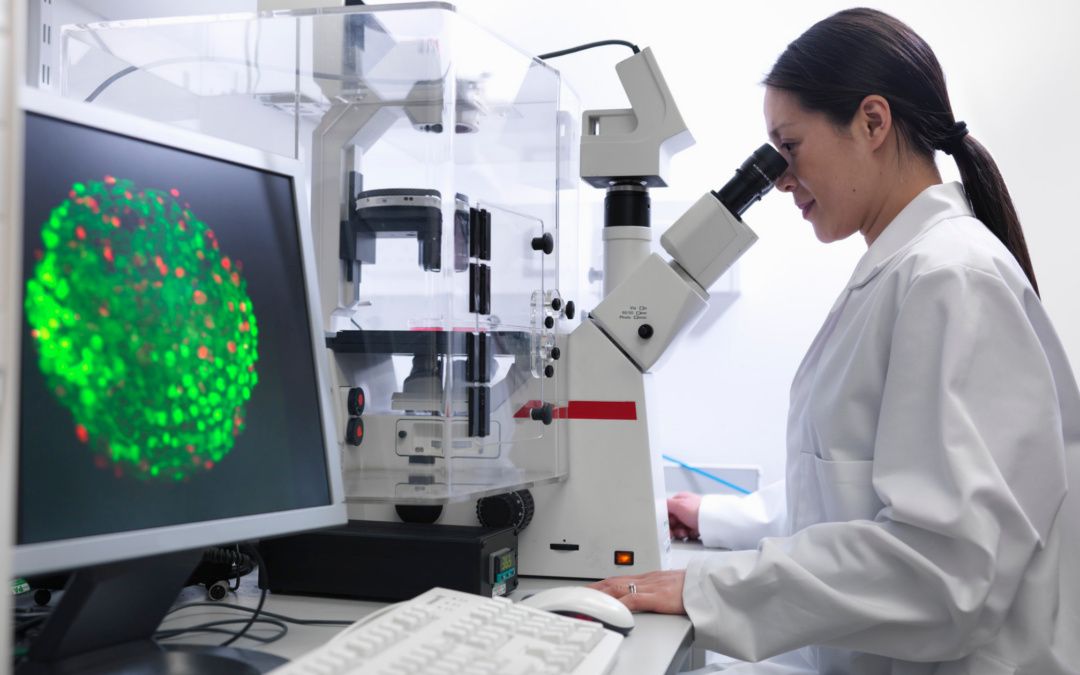
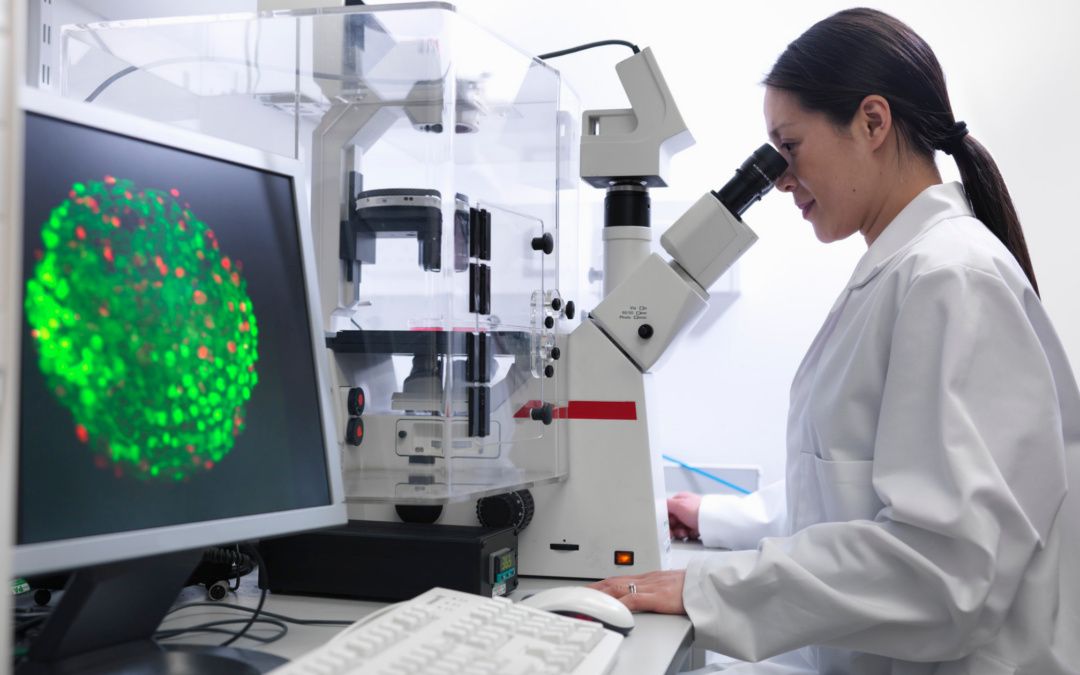
Regenerative medicine is a field of medicine that uses the body’s own cells and tissues to heal injuries and medical conditions. In the treatment of cancer the cells are used in immunotherapy, which involves modifying patient’s cells to fight the disease. In the field of orthopedics, regenerative medicine specialists use the patient’s own blood cells, bone marrow or adipose tissue to help the body boost its own natural healing properties. These are known as orthobiologics.
At the present time, FDA allows the use of autologous orthobiologics —which means the tissue or cells used must come from the same patient. Donor products are not allowed to be used in clinical setting unless it is used under the purview of a clinical trial. Read here on the FDA guidance on the use of human cells and tissues.
Cell-based Treatments for Orthopedic Conditions
There are two types of cell-based therapies that can be used to treat orthopedic conditions:
Bone Marrow Aspiration Concentrate (BMAC): Bone marrow-derived cells are collected from the back of the pelvic bone. The marrow contains mesenchymal stem cells which have the ability to renew themselves and differentiate into bone, tendon, cartilage and muscle cells. These make them an ideal therapy for treating orthopedic injuries such as tendon tears, worn cartilage, and degenerated disc disease. BMAC also contains important therapeutic cells, growth factors and proteins that stimulate the body’s natural ability to improve circulation, decrease inflammation and heal injured tissues.
Micro-fragmented Adipose Tissue (fat) Cells: Adipose-derived cells are collected from a fat sample usually from the buttock or abdomen. There is minimal manipulation of the tissue with no enzymatic digestion or addition of other biological or pharmacological agents. Fat or adipose tissue is rich in healing cells like mesenchymal stem cells or MSCs, growth factors and other proteins that can assist in healing tissues.
Why Consider Cell-Based Therapies?
There is increasing body of clinical research that demonstrates the safety and efficacy of Cell based therapies. A recent comprehensive report 1 based on actual clinical data collected from 65 physicians at 43 clinics in 25 states revealed that seventy percent of the patients treated with adipose tissue therapy reported a meaningful reduction in pain at 12 months following treatment and sixty-one percent of the patients treated with bone marrow aspirate reported a meaningful reduction in pain at12 months following treatment.
Micro-fragmented adipose tissue or bone marrow aspirate concentrate is a non-surgical treatment option that does not involve incisions, general anesthesia, hospitalizations or lengthy rehabilitation stays. This is an outpatient procedure performed in a doctor’s clinic using only local anesthesia.
Patients considering cell-based therapies should do their research in ensuring they get the best treatment. There are several important factors that can impact the effectiveness of these treatments. These include:
- Cellular product preparation: The patient’s bone marrow or fat tissue must be processed using FDA compliant devices and protocols. It must be prepared in a safe and sterile environment by medical personnel who are trained in the proper handling of these tissues.
- Delivery: The procedure must be performed by skilled physicians who are properly trained in this field. They must be able to perform these highly specialized injection techniques using imaging guidance to ensure that the cellular products are delivered to the site of injury.
- Experience: The field of regenerative medicine is changing daily and there are a limited number of specialists around the country who have the experience and technology to perform cell-based orthopedic treatments safely and effectively. Dr. Mary A. Ambach and Dr. Chris Rogers have decades of experience in using regenerative therapies and are nationally recognized experts in this field.
1Databiologics. An Overview of Regenerative Treatments for Orthopedic Conditions. 2021 Outcomes Report.

Nov 5, 2021
Prolotherapy, also known as proliferative therapy, is a treatment used to boost the body’s own natural healing capabilities to reduce inflammation, stimulate proliferation of injured tissue and relieve pain.
This is a minimally invasive therapy that involves injection of natural solutions to the injured tissue to stimulate healing. The main ingredient in the injection is dextrose, a sugar solution, which acts as an irritant to the body. The body reacts to the dextrose by stimulating repair and activating its natural healing abilities. The patient experiences relief as the injured tissue strengthens and heals.
What Conditions Can Prolotherapy Treat?
Prolotherapy can be used to treat any number of orthopedic conditions including:
- Osteoarthritis
- Ligament sprains
- Ligament laxity
- Tennis elbow
- Tendinopathy
- Sacroiliac joint ( SI joint) dysfunction
- Achilles tendinopathy
What Does Prolotherapy Entail?
Your physician will first complete an appropriate clinical evaluation and diagnostic testing to determine if you are a good candidate for prolotherapy. The procedure is a minimally invasive procedure performed in a medical clinic using local anesthesia. You may be asked to discontinue anti-inflammatory medications 3-5 days prior to the procedure. The procedure is performed using ultrasound or fluoroscopic guidance for precise localization of target and delivery of the solution. A small needle is used to inject the prolotherapy solution to the injured area using imaging guidance. Depending on the extent of the injury, a series of injections performed a few weeks apart may be needed for a successful treatment. You will be asked to take it easy for a few days and return to normal activity and exercises after 3-5 days. The procedure is very well tolerated with no downtime.
How Effective is This Type of Therapy?
Prolotherapy is a proven treatment that has been in use for more than 80 years and is practiced by physicians around the world. A review in the US National Library of Medicine of the National Institutes of Health evaluated 32 studies on dextrose prolotherapy for chronic musculoskeletal pain. It concluded that “dextrose prolotherapy has been demonstrated to be efficacious and should be considered as a treatment for pain and dysfunction associated with chronic musculoskeletal conditions, particularly tendinopathies and osteoarthritis.”[i]
A good review of prolotherapy treatments can be found here and here.
To learn more about SDOMG and how they have successfully utilized prolotherapy for more than three decades, fill out the form below:
Drs. Mary A. Ambach and Chris Rogers of San Diego Orthobiologics Medical Group have successfully treated hundreds of patients with prolotherapy and other cell-based treatments for more than three decades. Their state -of- the- art facility in Carlsbad offers the most advanced Regenerative Medicine treatments in San Diego with the highest level of safety and efficacy.
[i] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938120/

Aug 2, 2021
Dr. Mary Ambach lectures to physicians, orthopedic surgeons and other orthopedic practitioners on the use of Platelet Rich Plasma and Stem Cell Therapies for the Spine.
Dr. Ambach is one of the esteemed instructors in this Orthobiologic seminar who taught physicians on how to perform regenerative injections and diagnostic musculoskeletal ultrasound scans.
Dr. Ambach has served as faculty and speaker at regenerative conferences in and outside of the country. She has mentored many doctors all over the world in innovative procedures using cell therapies from our own bodies to heal our own orthopedic injuries.