Jan 23, 2026
Platelet-rich plasma (PRP) injections have gained attention as a regenerative treatment option for patients seeking relief from joint, tendon, ligament, and soft tissue pain. Often used in orthopedics, sports medicine, and pain management, PRP offers a minimally invasive approach designed to support the body’s natural healing processes. If you’re considering PRP therapy, understanding how it works, what it treats, and what to expect can help you make an informed decision.
What Are PRP Injections?
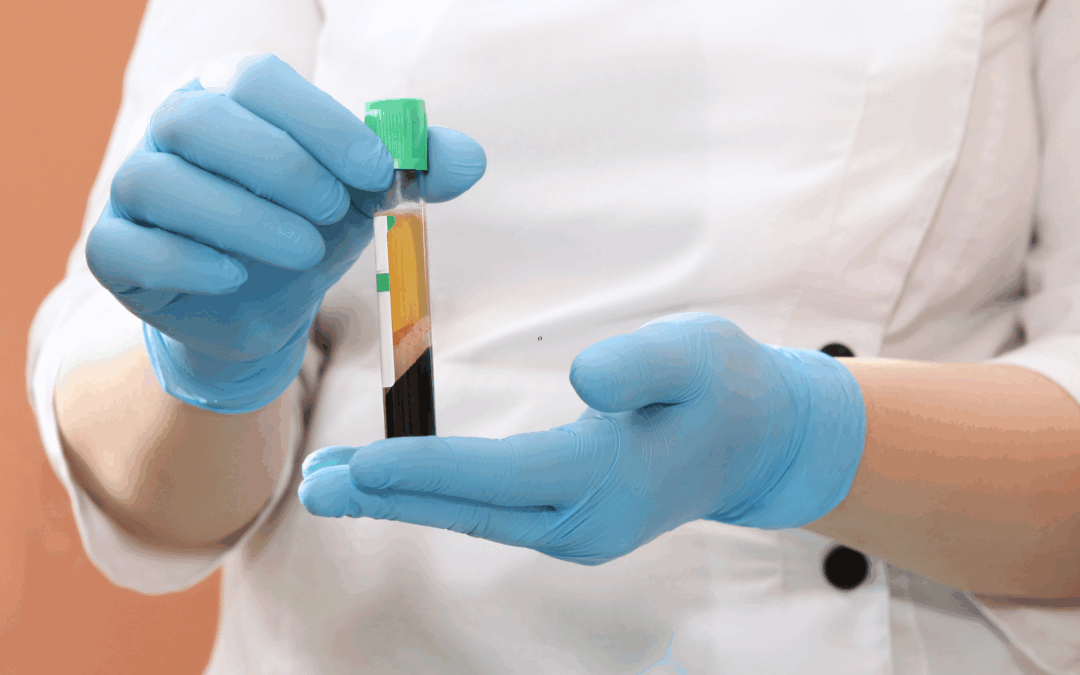
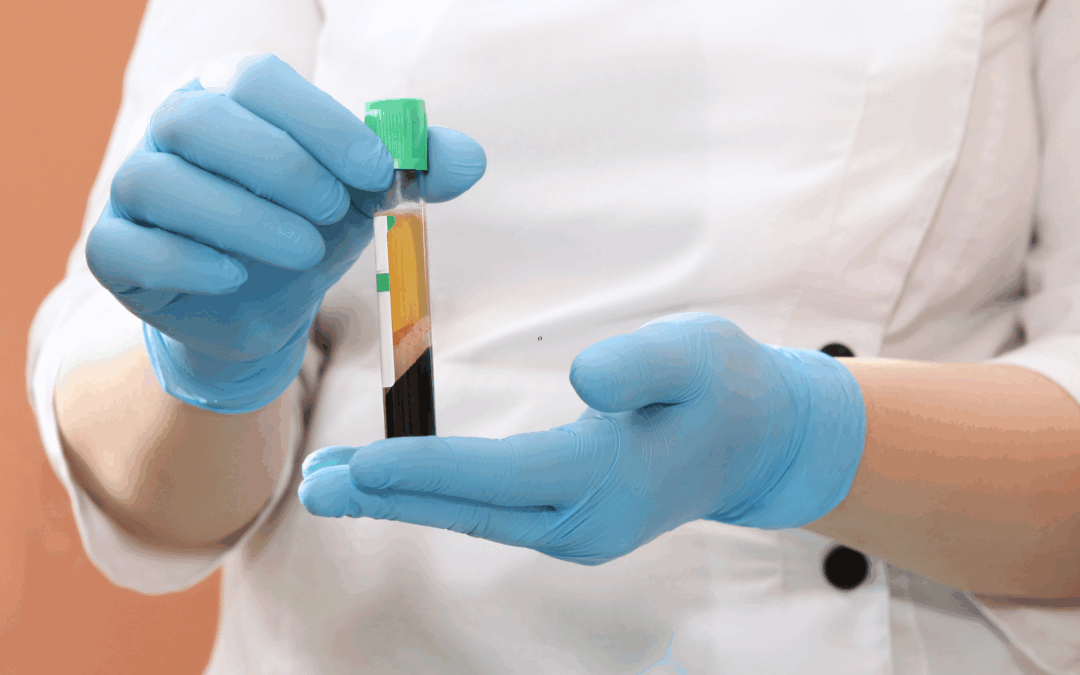
PRP stands for platelet-rich plasma. Platelets are a natural component of blood best known for their role in clotting, but they also contain growth factors that support tissue repair.
During a PRP procedure:
- A small amount of the patient’s blood is drawn
- The blood is spun in a centrifuge to concentrate the platelets
- The platelet-rich portion is injected into the targeted area
Because PRP is derived from the patient’s own blood, the risk of allergic reaction or rejection is extremely low.
How PRP Supports Healing
PRP works by delivering a high concentration of growth factors directly to injured or degenerative tissue. These growth factors may:
- Promote tissue repair
- Reduce inflammation
- Support collagen production
- Encourage cellular regeneration
Rather than simply masking pain, PRP aims to improve the underlying tissue environment to support longer-term healing.
Conditions Commonly Treated with PRP
PRP injections may be recommended for a variety of musculoskeletal conditions, including:
- Knee, hip, and shoulder osteoarthritis
- Tendon injuries (such as tennis elbow or Achilles tendinopathy)
- Ligament sprains
- Chronic joint pain
- Muscle injuries
- Certain spine-related soft tissue conditions
PRP is often considered when conservative treatments like physical therapy or medications have not provided sufficient relief.
What to Expect During and After Treatment
PRP injections are typically performed in an outpatient setting and usually take less than an hour.
After the procedure:
- Mild soreness or swelling at the injection site is common
- Patients are often advised to limit strenuous activity for several days
- Pain relief and functional improvement may develop gradually over weeks
Because PRP stimulates a biological healing response, results are not immediate. Some patients may require a series of injections depending on the condition being treated.
Is PRP Right for Everyone?
While PRP is generally safe, it may not be appropriate for all patients. Factors such as:
- Severity of tissue damage
- Overall health
- Blood disorders or active infections
- Treatment goals
should be discussed with a qualified medical provider. PRP is not a replacement for surgery in severe structural damage, but it may help delay or reduce the need for more invasive procedures.
It’s also important to note that PRP is considered a biologic therapy, and coverage varies because it is not universally approved by U.S. Food and Drug Administration for all indications.
PRP vs. Steroid Injections
Unlike corticosteroid injections, which primarily reduce inflammation and pain temporarily, PRP aims to support tissue repair. Steroids may provide faster relief but can weaken tissues with repeated use. PRP may take longer to show results but is often chosen for its regenerative potential.
Final Thoughts
PRP injections represent an evolving approach in regenerative and pain medicine, offering patients a minimally invasive option that works with the body’s natural healing abilities. While results vary, many patients find PRP to be a valuable part of a comprehensive, non-surgical treatment plan.
If you’re experiencing ongoing joint or soft tissue pain, a consultation with a pain management or regenerative medicine specialist can help determine whether PRP is an appropriate option for you.
Dec 24, 2025
Tendon injuries and chronic tendon degeneration — often called tendinopathy — are common yet stubbornly difficult to treat. From athletes pushing through pain to older adults coping with age-related wear, tendon issues can severely limit movement and quality of life. Traditional approaches like rest, physical therapy, anti-inflammatory medications, or surgery remain standard, but many people still struggle with lingering pain and functional limitations. Thankfully, emerging regenerative medicine approaches offer new hope — and a fundamentally different way of thinking about healing.
What Makes Tendons Hard to Heal?
Unlike other tissues, tendons have a poor blood supply, limiting their natural healing ability. When injured, tendons often form scar tissue rather than regenerating healthy tendon fibers, which can lead to chronic pain and repeated injury cycles. Aging, repetitive strain, and certain systemic conditions can worsen this process, making degeneration a long-lasting problem.
Regenerative Medicine: Healing Over Scarring
Regenerative medicine offers therapies that go beyond simply reducing symptoms. Instead, these treatments aim to stimulate the body’s own healing mechanisms, potentially leading to more complete tissue repair.
Here are some of the most studied and promising options:
1. Platelet-Rich Plasma (PRP) Therapy
PRP involves drawing a patient’s own blood, concentrating the platelets, and then injecting this platelet-rich plasma into the injured tendon. Platelets release growth factors that may help stimulate tendon cell activity, reduce inflammation, and support repair. PRP is one of the most widely used regenerative treatments for tendon injuries and is often offered as an outpatient procedure with minimal downtime.
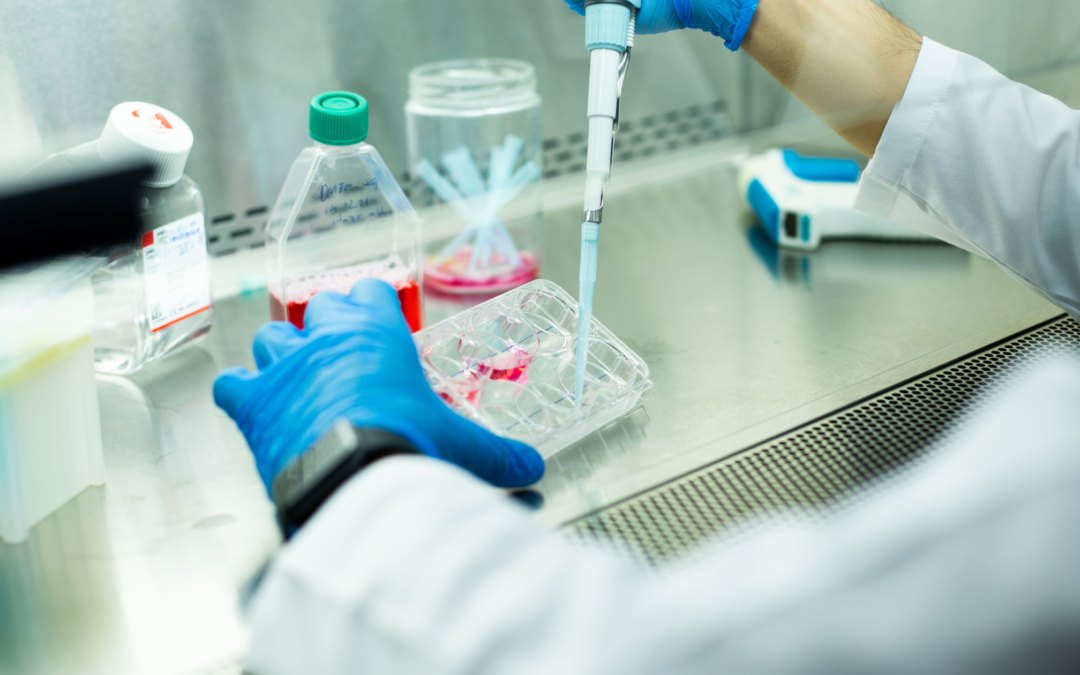
2. Stem Cell-Based Therapies
Mesenchymal stem cells (from bone marrow or adipose tissue) are being researched for their ability to differentiate into tendon-like cells and secrete healing signals. Early studies suggest they could help modulate inflammation and support regeneration. Although clinical evidence continues to evolve and large, high-quality trials are still needed, many researchers view stem cells as a key frontier in tendon repair science.
3. Next-Generation Blood Factor Treatments
Beyond traditional PRP, newer approaches aim to isolate specific growth factors or concentrate regenerative signals more precisely. Plasma-Derived Factor treatments (like PDF-FD) extract and concentrate key proteins from blood, then deliver them directly to the injured site — potentially enhancing healing responses.
Other Frontiers: Biomaterials & Tissue Engineering
Researchers are also looking at biomaterials, scaffolds, and guided tissue engineering as ways to support tendon regeneration structurally and biologically. These approaches use engineered materials to provide a framework for tendon cells to grow — which, in theory, could rebuild tissue more like the original tendon. Although many of these are still in early stages, they represent exciting future directions.
What to Know Before Considering Regenerative Treatments
- Evidence varies: While some regimens are backed by clinical research, others are still experimental. The strength of evidence for effectiveness differs across therapies, and not all treatments are universally accepted by mainstream medical societies.
- Regulation and safety: Some regenerative therapies are regulated, others are offered at clinics without standardized oversight. Discuss risks, benefits, and alternatives with a qualified provider.
- Not a magic bullet: Regenerative treatments are most effective when combined with physical therapy, lifestyle changes, and proper loading programs to support tendon health.
Conclusion
Tendon injuries and degeneration don’t have to be resigned to “rest and wait.” The emerging world of regenerative medicine showcases promising paths to enhance healing, stimulate regeneration, and restore function — even for chronic tendon issues. As research advances and clinical evidence grows, these biologic solutions may reshape how we approach tendon care in the years ahead.
Nov 21, 2025
Musculoskeletal pain can disrupt work, daily activities, hobbies, and sleep. When injuries or chronic conditions don’t improve with rest or basic treatments, many patients assume surgery is the next step. But today, several advanced non-surgical regenerative therapies can help the body repair damaged tissue, reduce inflammation, and restore function—often without the risks or downtime of an operation.
These modalities aim to support the body’s natural healing processes, making them valuable options for athletes, active individuals, and anyone seeking to avoid surgery.
What Are Regenerative Therapies?
Regenerative medicine focuses on enhancing or accelerating tissue repair. Unlike medications that primarily mask symptoms, regenerative therapies work at the source of the problem. They can support healing in muscles, tendons, ligaments, joints, and even nerve-related structures.
These treatments are minimally invasive and often performed in-office using imaging guidance for precision.
Common Musculoskeletal Conditions That Benefit from Regenerative Care
Regenerative therapies may help with:
-
Tendon injuries (tennis elbow, Achilles tendonitis, rotator cuff injuries)
-
Ligament sprains
-
Mild to moderate osteoarthritis
-
Muscle strains and chronic myofascial pain
-
Plantar fasciitis
-
Joint instability
-
Overuse injuries
-
Degenerative disc or facet-related spine pain (in selected cases)
Key Non-Surgical Regenerative Modalities
Platelet-Rich Plasma (PRP)
PRP leverages your own concentrated platelets, which contain growth factors that stimulate healing. A small sample of your blood is processed, then injected into the injured area. PRP is commonly used for tendon tears, arthritis, and chronic joint pain.
Benefits:
Platelet-Rich Fibrin (PRF)
PRF is similar to PRP but processed more gently, creating a fibrin matrix that slowly releases growth factors over time. This can provide a more sustained healing effect for hard-to-treat conditions.
Stem Cell–Rich Biologic Therapies
While true stem cell procedures are highly regulated, many clinicians use bone marrow concentrate or other cell-rich biologics to support regeneration in damaged tissues.
Used for:
Prolotherapy
This involves injecting a natural irritant, often dextrose, to stimulate the body’s healing response. It helps strengthen ligaments and tendons and can improve joint stability that contributes to chronic pain.
Benefits:
Why Patients Choose Regenerative Therapies
-
Avoiding surgery and downtime
-
Faster recovery compared to surgical options
-
Reduction in chronic inflammation
-
Long-term improvement in pain and function
-
Potential to treat underlying causes rather than masking symptoms
When to Consider Regenerative Treatments
You may be a good candidate if you:
-
Have persistent pain despite physical therapy, activity modification, or medications
-
Have been told surgery is an option but want to avoid or delay it
-
Prefer a more natural, biologic approach to healing
-
Want to return to activities sooner
-
Have soft tissue, joint, or mild spine-related pain
A pain or musculoskeletal specialist can help determine which regenerative option aligns with your condition and goals.
Final Thoughts
Non-surgical regenerative therapies are transforming how we treat musculoskeletal pain and injury. By activating and supporting the body’s own healing mechanisms, these treatments offer a path to recovery that is less invasive, more natural, and often highly effective.
If you’re dealing with ongoing pain or an injury that isn’t healing as expected, regenerative medicine may offer the solution you’ve been looking for.

Jun 18, 2025
Regenerative medicine has emerged as a groundbreaking frontier in healthcare, offering hope to those suffering from chronic pain, degenerative conditions, and tissue injuries. This field harnesses the body’s natural healing abilities to restore or replace damaged tissues, reduce inflammation, and improve function. From platelet-rich plasma (PRP) therapy to stem cell treatments, regenerative therapies are transforming how we approach recovery and long-term wellness.
But not everyone is an ideal candidate. Understanding whether regenerative medicine is right for you is crucial to getting the best results. If you’ve been considering this innovative approach, here are five signs you might be a good candidate for regenerative medicine treatments.
Signs You Are a Good Candidate for Regenerative Medicine Treatments
1. You Have a Musculoskeletal Injury or Chronic Joint Pain
Regenerative medicine has shown particular promise in treating orthopedic conditions, especially those involving joints, tendons, ligaments, and cartilage. Whether it’s a sports injury like a torn meniscus or rotator cuff, or chronic issues such as osteoarthritis, regenerative therapies can help repair damaged tissues and reduce inflammation.
If you’ve been struggling with:
- Knee, shoulder, or hip pain
- Tendonitis or bursitis
- Cartilage degeneration
- Minor ligament tears
…you may be a strong candidate for treatments like stem cell therapy or PRP injections. These approaches aim to accelerate the body’s natural healing process, potentially helping you avoid invasive surgery or long-term use of pain medications.
Bonus Tip: If you’re in the early to moderate stages of arthritis or injury, you’re more likely to benefit from regenerative treatments than if your joint is severely damaged or completely worn down.
2. Conservative Treatments Haven’t Worked
If you’ve already tried physical therapy, rest, steroid injections, and anti-inflammatory medications without success, regenerative medicine may be your next step. Many patients turn to regenerative therapies when they reach a plateau in traditional treatment or want to avoid more aggressive interventions like surgery.
Patients often choose regenerative medicine because:
- They want a more natural approach to healing.
- They are looking for a longer-term solution instead of a temporary fix.
- They’ve exhausted other non-surgical methods without lasting relief.
It’s important to understand that regenerative treatments are not a quick fix. They work by stimulating the body’s healing mechanisms, which may take weeks or even months to show full results. But for many, the wait is worth the long-term improvement.
3. You’re in Generally Good Health
Your overall health plays a significant role in determining whether regenerative medicine will be effective. While these therapies are minimally invasive and low-risk, your body needs to be in a relatively good state to respond optimally to treatment.
Ideal candidates typically:
- Are not smokers or are willing to quit (smoking impairs healing).
- Are not severely overweight or are actively working on weight management.
- Have stable blood sugar levels (uncontrolled diabetes can interfere with cell healing).
- Are free from active infections or cancer.
Good health doesn’t mean you have to be an elite athlete—it just means your body can efficiently participate in the healing process. If you’re not sure whether your health status qualifies, a qualified regenerative medicine specialist can help evaluate your risk factors and determine the safest approach.
4. You Want to Avoid Surgery
Surgery isn’t always the best or most desirable option, especially when it comes with extended downtime, risks, and unpredictable outcomes. Regenerative medicine appeals to many people because it offers a non-surgical alternative that may still provide meaningful relief and functional improvement.
If you’re considering surgery but:
- Want to try a less invasive option first
- Need to avoid lengthy recovery due to work or lifestyle
- Have already had one surgery and don’t want another
- Have been told you’re not an ideal surgical candidate
…then regenerative therapies may be an appropriate avenue to explore.
For example, some patients with degenerative disc disease or mild meniscus tears can avoid or delay surgery through stem cell or PRP treatments, which aim to reduce pain and improve mobility naturally. While not a guaranteed substitute for surgery, these therapies may help manage symptoms and extend the life of your joints or tissues.
5. You’re Committed to a Holistic Recovery Process
Regenerative medicine is part of a bigger picture—one that includes lifestyle, nutrition, physical therapy, and patient mindset. The most successful outcomes often come from individuals who are proactive, disciplined, and patient.
Ask yourself:
- Are you willing to follow post-treatment care recommendations?
- Will you commit to physical therapy or exercise as advised?
- Are you open to dietary or behavioral changes that support healing?
- Do you have realistic expectations about gradual improvement?
These treatments are not magic bullets. They’re catalysts for your body’s natural healing systems, and that process takes time and effort. Being engaged and proactive in your care significantly increases your chances of a positive outcome.
A Final Thought: Not Everyone is a Candidate—And That’s Okay
Regenerative medicine is not a one-size-fits-all solution. While it holds exciting promise for many, there are circumstances where it might not be the best choice. Severe joint deformities, complete tissue loss, or advanced systemic diseases may limit the effectiveness of these therapies.
That’s why a comprehensive evaluation with a regenerative medicine specialist is critical. A qualified provider will assess your medical history, imaging, lifestyle, and goals to determine whether you’re likely to benefit—and they won’t recommend it unless they genuinely believe it can help you.
Conclusion
Regenerative medicine offers a path toward healing that emphasizes the body’s innate ability to recover, repair, and rejuvenate. If you’re dealing with persistent joint or tendon issues, have tried conservative treatments without success, are in good overall health, and are motivated to avoid surgery through a more natural and holistic route, you might be an excellent candidate.
The best first step? Schedule a consultation with a trusted provider specializing in regenerative therapies at San Diego Orthobiologics Medical Group. With a personalized evaluation and guidance, you can discover whether this innovative treatment could be the breakthrough your body has been waiting for.
Interested in learning more about regenerative medicine?
Our clinic offers in-depth assessments and cutting-edge regenerative therapies tailored to your needs. Contact us today to book a consultation and take the next step toward lasting relief and better function—naturally.

May 30, 2025
In the high-stakes world of sports, injury recovery time can define the trajectory of an athlete’s career. Whether it’s a torn ligament, chronic tendonitis, or a nagging joint issue, athletes are always seeking faster and more effective ways to heal and return to peak performance. This is where regenerative medicine, particularly Platelet-Rich Plasma (PRP) and Bone Marrow Aspirate Concentrate (BMAC), has emerged as a transformative solution.
These innovative therapies leverage the body’s own biological resources to accelerate tissue repair, reduce inflammation, and minimize downtime. In this post, we’ll delve into how PRP and BMAC are being used to help athletes recover faster from injuries and why they’re gaining popularity in sports medicine.
What is Regenerative Medicine?
Regenerative medicine refers to treatments that aim to restore normal function by repairing or regenerating damaged tissues or organs using the body’s own healing mechanisms. Unlike traditional treatments that manage symptoms or rely on surgical intervention, regenerative therapies work at the cellular level to enhance the natural healing process.
Among the most widely accepted and commonly used forms of regenerative medicine in athletic recovery are Platelet-Rich Plasma (PRP) and Bone Marrow Aspirate Concentrate (BMAC).
Platelet-Rich Plasma (PRP): Supercharging the Body’s Healing Process
PRP therapy involves concentrating platelets from a patient’s own blood and injecting them into the injured area. Platelets are rich in growth factors—biological signals that stimulate tissue repair and regeneration.
How PRP Works
- Blood Collection: A small amount of the athlete’s blood is drawn, typically from the arm.
- Centrifugation: The blood is spun in a centrifuge to separate platelets from other components.
- Injection: The resulting PRP—plasma with a high concentration of platelets—is injected directly into the injured tissue under ultrasound guidance.
PRP Applications in Sports Injuries
PRP is used extensively for musculoskeletal injuries common in sports, including:
- Tendonitis (e.g., tennis elbow, Achilles tendonitis)
- Ligament sprains (e.g., MCL sprains)
- Muscle tears
- Joint degeneration (e.g., mild osteoarthritis)
Benefits of PRP for Athletes
- Accelerated Healing: PRP delivers concentrated growth factors to the injury site, promoting faster tissue regeneration.
- Reduced Inflammation: The therapy helps modulate the inflammatory response, which can reduce pain and swelling.
- Minimally Invasive: As an injection-based treatment, PRP avoids the trauma of surgery and its associated risks.
- Shorter Downtime: Many athletes return to training and competition sooner than with traditional rehabilitation alone.
Bone Marrow Aspirate Concentrate (BMAC): A Rich Source of Healing Cells
Bone Marrow Aspirate Concentrate (BMAC) is another autologous (self-derived) regenerative therapy. It involves aspirating bone marrow—typically from the iliac crest (hip bone)—and concentrating the healing components for injection into injured tissues.
What’s in BMAC?
BMAC is rich in:
- Platelets: Similar to PRP, these deliver growth factors that aid in healing.
- White blood cells: Important for modulating inflammation and fighting infection.
- Progenitor cells: These assist in the repair and regeneration of damaged tissue, especially in bone and cartilage injuries.
How BMAC Works
- Harvesting: Bone marrow is collected using a minimally invasive aspiration procedure.
- Processing: The marrow is processed to concentrate the regenerative components.
- Injection: The final concentrate is injected into the site of injury.
BMAC Applications in Athletic Recovery
BMAC is especially useful in treating:
- Cartilage injuries
- Joint degeneration
- Non-healing bone fractures
- Chronic tendon and ligament injuries
Benefits of BMAC for Athletes
- Deep Tissue Repair: BMAC is effective for more complex or severe injuries, especially those involving cartilage and bone.
- One-Time Treatment: In many cases, a single BMAC injection can provide significant improvement.
- Natural and Autologous: As with PRP, BMAC uses the athlete’s own biological material, minimizing risk of rejection or complications.
- Enhanced Recovery: Athletes often experience reduced pain, improved function, and quicker return to play.
Clinical Evidence
BMAC has been studied for its potential in treating cartilage defects and bone injuries. A 2016 clinical trial published in Orthopaedic Journal of Sports Medicine showed that athletes with knee cartilage lesions treated with BMAC experienced meaningful improvements in function and pain relief.
PRP vs. BMAC: Which is Better for Athletic Injuries?
While both PRP and BMAC are powerful tools in regenerative medicine, they serve different roles depending on the nature and severity of the injury.
| Aspect |
PRP |
BMAC |
| Source |
Blood |
Bone marrow |
| Best For |
Soft tissue injuries, mild arthritis |
Bone/cartilage injuries, chronic damage |
| Processing Complexity |
Low |
Moderate to high |
| Healing Potential |
Moderate |
Higher (especially for deeper injuries) |
| Invasiveness |
Minimally invasive (blood draw) |
Slightly more invasive (bone aspiration) |
In many sports medicine clinics, practitioners assess the injury type, severity, and the athlete’s goals to determine which therapy—or combination—is most suitable.
The Athlete’s Perspective: Real-World Impact
Athletes from every discipline, from weekend warriors to Olympic gold medalists, are increasingly turning to PRP and BMAC to speed up recovery. High-profile sports figures like Tiger Woods, Rafael Nadal, and Kobe Bryant have reportedly used PRP therapy to overcome injuries and return to elite competition.
For athletes, the primary appeal of these treatments lies in the combination of effectiveness and reduced recovery time. In a world where every game, match, or race matters, shaving weeks off a recovery timeline can make a critical difference.
Limitations and Considerations
While PRP and BMAC are promising, they’re not miracle cures. Effectiveness can vary based on:
- Type and chronicity of injury
- Overall health and age of the athlete
- Technique and quality of the preparation
Additionally, these treatments may not be covered by insurance and can be costly, though many athletes see them as worthwhile investments in their careers and long-term joint health.
Conclusion
Regenerative medicine is reshaping the future of sports injury recovery. PRP and BMAC stand at the forefront, offering biologically-based, minimally invasive options to accelerate healing and reduce downtime for athletes of all levels. As research continues and technology advances, the integration of these therapies into mainstream sports medicine is expected to grow—giving injured athletes a faster, safer path back to the game.
Whether you’re a professional athlete or an active individual looking to get back on your feet, PRP and BMAC offer compelling alternatives to surgery and long-term medications. Always consult with a qualified sports medicine specialist to determine the best course of action tailored to your specific condition and goals.
Apr 23, 2025
Arthritis affects over 58 million adults in the United States alone, making it a leading cause of disability and pain. Traditionally, treatment options have focused on symptom management through medications, physical therapy, and, in severe cases, joint replacement surgery. However, recent advances in regenerative medicine are changing the landscape of arthritis care by offering promising, non-surgical alternatives that aim to repair and restore damaged tissues.
In this post, we’ll explore the latest regenerative medicine techniques used to treat arthritis, how they work, and why they’re generating excitement among physicians and patients alike.
Understanding Arthritis and Its Impact
Arthritis is not a single disease but a term that covers more than 100 different types of joint conditions. The most common forms are osteoarthritis (OA) and rheumatoid arthritis (RA):
- Osteoarthritis is a degenerative joint disease where the cartilage that cushions bones wears down over time.
- Rheumatoid arthritis is an autoimmune condition where the immune system attacks the synovial lining of the joints, causing inflammation and tissue damage.
Regardless of the type, arthritis often leads to joint pain, stiffness, decreased mobility, and a diminished quality of life.
Why Patients Seek Non-Surgical Options
Joint replacement surgery, while effective, comes with risks: infection, blood clots, lengthy recovery periods, and even the potential for implant failure over time. Many patients are not ready—or suitable candidates—for surgery and seek less invasive options to manage symptoms and improve joint function.
That’s where regenerative medicine steps in.
What Is Regenerative Medicine?
Regenerative medicine harnesses the body’s natural healing mechanisms to repair or replace damaged tissues, including cartilage, ligaments, tendons, and even bone. These treatments aim to not only reduce symptoms but also to slow or potentially reverse the progression of arthritis.
The most promising regenerative therapies for arthritis include:
- Platelet-Rich Plasma (PRP) Therapy
- Cell-Based Therapy
- Prolotherapy
Let’s break down each of these innovative techniques.
-
Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves drawing a small amount of the patient’s blood, processing it to concentrate the platelets, and then injecting this platelet-rich plasma into the affected joint.
How It Works:
Platelets contain growth factors that help stimulate tissue regeneration and reduce inflammation. When injected into an arthritic joint, PRP can:
- Promote cartilage healing
- Decrease pain and stiffness
- Improve joint function
Clinical Evidence:
Studies have shown PRP can be more effective than corticosteroids or hyaluronic acid injections in relieving knee osteoarthritis symptoms. Results are typically seen within weeks and can last for several months or even over a year.
-
Cell-Based Therapy
Stem cells are undifferentiated cells capable of transforming into various tissue types, including cartilage. In arthritis treatment, mesenchymal stem cells (MSCs) are commonly harvested from a patient’s bone marrow or adipose (fat) tissue and injected into the joint.
How It Works:
Once inside the joint, stem cells can:
- Stimulate repair of damaged cartilage
- Modulate inflammation
- Recruit other cells to aid in tissue regeneration
Clinical Evidence:
Early studies have reported significant improvements in pain, mobility, and cartilage thickness following stem cell injections. While more research is needed to establish standardized protocols, the outlook is encouraging—especially for early to moderate osteoarthritis.
-
Prolotherapy
Prolotherapy is a regenerative injection technique that involves injecting a natural irritant—often a dextrose (sugar) solution—into the joint or surrounding ligaments and tendons.
How It Works:
The solution triggers a localized inflammatory response, prompting the body to send healing cells to the area. Over time, this can strengthen connective tissues and stabilize the joint.
Who It’s For:
Prolotherapy is particularly effective for patients with joint instability, ligament laxity, or early-stage arthritis. It’s less commonly used for severe osteoarthritis but can still play a role as part of a broader regenerative plan.
Benefits of Regenerative Medicine for Arthritis
- Minimally Invasive: Most procedures are outpatient and involve little to no downtime.
- Reduced Dependence on Medications: Patients may rely less on NSAIDs, opioids, or corticosteroids.
- Slowed Disease Progression: Some therapies show the potential to halt or even reverse cartilage loss.
- Improved Quality of Life: Many patients report enhanced mobility, reduced pain, and greater participation in daily activities.
Important Considerations
Not a One-Size-Fits-All Solution
Regenerative therapies work best in the early to moderate stages of arthritis. They may not be as effective for patients with advanced joint deterioration.
Costs and Coverage
These treatments are often not covered by insurance and can range from a few hundred to several thousand dollars per session. However, many patients find the cost worthwhile for the benefits they experience.
Choose a Qualified Provider
It’s essential to seek care from physicians who specialize in regenerative medicine and follow best practices for safety, preparation, and delivery. Improper technique or unregulated products can result in complications.
The Future of Arthritis Treatment
Regenerative medicine is rapidly evolving. As research deepens and technology advances, these therapies may soon become mainstream components of arthritis care. Clinical trials are underway to determine long-term outcomes, best candidates, and optimal treatment protocols.
What’s exciting is that these approaches shift the paradigm from merely managing symptoms to actively promoting healing—a revolutionary step for the millions living with arthritis.
Final Thoughts
If you’re struggling with arthritis pain and looking for alternatives to surgery, regenerative medicine offers a promising path forward. From PRP to stem cells and beyond, these innovative techniques can help restore joint health, improve function, and reduce your reliance on medications.
Always consult a qualified healthcare professional to determine which therapy, if any, is right for you. With the right approach, living well with arthritis is not only possible—it’s becoming increasingly probable.
Interested in learning more about regenerative treatments? Talk to a regenerative medicine specialist or rheumatologist to explore your options based on your specific type of arthritis and stage of progression.