Feb 6, 2026
Joint preservation focuses on protecting and maintaining the natural function of joints for as long as possible. Instead of immediately resorting to joint replacement surgery, joint preservation aims to slow or halt joint degeneration, reduce pain, and improve mobility through early diagnosis and targeted treatments.
As arthritis and joint degeneration often develop gradually, early intervention plays a critical role in maintaining joint health. By addressing symptoms and structural changes early, patients may be able to delay—or even avoid—the need for surgical joint replacement.
What Causes Early Joint Degeneration?
Joint degeneration can occur for several reasons, and it often begins long before noticeable symptoms develop. Some of the most common contributing factors include:
- Osteoarthritis: The most common form of arthritis caused by wear and tear of cartilage.
- Previous Injuries: Sports injuries, ligament tears, fractures, or joint dislocations can accelerate degeneration.
- Repetitive Stress: Jobs or activities that place consistent strain on joints may lead to early damage.
- Inflammatory Conditions: Rheumatoid arthritis and other autoimmune diseases can affect joint tissues.
- Age and Genetics: Natural aging and family history both play a role in joint health.
- Excess Weight: Additional body weight places increased pressure on weight-bearing joints such as the knees and hips.
Understanding the underlying cause helps healthcare providers create a personalized joint preservation plan.
Recognizing Early Signs of Arthritis
Early arthritis symptoms can be subtle and are sometimes mistaken for normal aging or minor injury. Seeking medical evaluation when symptoms first appear can significantly improve treatment outcomes.
Common early warning signs include:
- Joint stiffness, especially in the morning or after inactivity
- Mild but persistent joint pain
- Swelling or tenderness around joints
- Decreased range of motion
- Clicking, grinding, or popping sensations in the joint
- Fatigue or discomfort during physical activity
If these symptoms persist or worsen over time, early intervention may help protect the joint from further deterioration.
Diagnostic Tools for Early Arthritis Detection
Accurate diagnosis is essential for effective joint preservation. Providers may use a combination of evaluation methods, including:
Physical Examination
Assessment of joint movement, stability, strength, and areas of pain.
Imaging Studies
- X-rays: Identify bone changes and cartilage loss.
- MRI: Detect soft tissue damage, cartilage injuries, and early joint degeneration.
- Ultrasound: Evaluate inflammation, fluid buildup, and soft tissue abnormalities.
Laboratory Testing
Blood tests may help identify inflammatory or autoimmune causes of joint pain.
Non-Surgical Joint Preservation Treatments
Many early arthritis cases can be managed effectively without surgery. Treatment plans often include a combination of therapies tailored to the patient’s condition and lifestyle.
Physical Therapy and Rehabilitation
Targeted exercises help strengthen muscles around the joint, improve flexibility, and enhance stability, which reduces strain on damaged joint structures.
Activity Modification
Adjusting daily activities or athletic movements can reduce repetitive joint stress while maintaining overall mobility and function.
Weight Management
Maintaining a healthy weight can significantly reduce pressure on joints, particularly in the knees, hips, and spine.
Medication Management
Anti-inflammatory medications and pain relievers may help control symptoms and improve comfort during daily activities.
Advanced Joint Preservation Procedures
When conservative treatments are not enough, minimally invasive and regenerative therapies may help support joint repair and healing.
Injection-Based Therapies
- Corticosteroid Injections: Reduce inflammation and provide temporary pain relief.
- Hyaluronic Acid Injections: Improve joint lubrication and mobility.
- Platelet-Rich Plasma (PRP): Uses the patient’s own blood components to promote healing and tissue repair.
Regenerative Medicine
Emerging regenerative therapies aim to stimulate the body’s natural healing processes to repair damaged tissues and slow joint degeneration.
Minimally Invasive Arthroscopic Procedures
In some cases, arthroscopy may be used to repair cartilage, remove damaged tissue, or correct joint alignment before advanced arthritis develops.
Lifestyle Strategies to Support Joint Preservation
Patients can play an active role in maintaining joint health through daily habits that support long-term mobility.
Helpful strategies include:
- Staying physically active with low-impact exercises such as swimming, cycling, or walking
- Practicing stretching and flexibility routines
- Using proper body mechanics during lifting or exercise
- Wearing supportive footwear
- Following an anti-inflammatory diet rich in whole foods, lean proteins, fruits, vegetables, and healthy fats
When Is Joint Replacement Necessary?
Joint replacement surgery may become necessary when:
- Joint damage is severe
- Pain significantly limits daily activities
- Conservative treatments no longer provide relief
- Mobility and quality of life are severely affected
The goal of joint preservation is not to eliminate joint replacement entirely but to delay it whenever possible, allowing patients to maintain their natural joint function longer.
The Importance of Early Arthritis Care
Early arthritis care focuses on proactive management rather than reactive treatment. Patients who seek evaluation and treatment at the first signs of joint discomfort often experience better outcomes, slower disease progression, and improved quality of life.
Healthcare providers specializing in joint preservation can develop personalized treatment plans designed to:
- Reduce inflammation and pain
- Improve joint stability and function
- Slow or prevent further joint damage
- Support long-term mobility and activity levels
Final Thoughts
Joint preservation and early arthritis care emphasize the importance of early diagnosis, conservative treatment, and proactive lifestyle changes. With modern medical advancements and individualized care plans, many patients can successfully manage arthritis symptoms and maintain active, healthy lives without immediate surgery.
If you are experiencing early joint pain, stiffness, or mobility limitations, seeking professional evaluation can help protect your joints and preserve long-term function.

Dec 5, 2025
As temperatures drop, many people notice their joints becoming stiff, achy, or more painful than usual. Winter weather can aggravate conditions like arthritis, tendon injuries, and chronic joint degeneration—making it harder to stay active and comfortable. While traditional treatments such as NSAIDs, bracing, and heat therapy offer temporary relief, patients looking for longer-term improvement often turn to regenerative medicine.
Here’s why winter is actually one of the best times to explore regenerative options like PRP (platelet-rich plasma), orthobiologics, and cell-based therapies.
Why Joints Hurt More in Winter
Many patients describe their joints as “weather predictors,” especially when cold air arrives. Several factors explain why winter intensifies joint discomfort:
1. Changes in Barometric Pressure
Dropping pressure can cause joint tissues to expand slightly, leading to increased stiffness or pain—especially in joints already affected by inflammation or degeneration.
2. Cold Muscles = Stiffer, Tighter Movement
Cold temperatures reduce muscle elasticity. This places extra strain on tendons, ligaments, and joints.
3. Reduced Activity Levels
Shorter days and cold weather reduce physical activity, which weakens supportive muscles and worsens joint mobility.
4. Increased Inflammation
For some individuals, cold stress increases inflammatory responses, intensifying pain in arthritic or injured joints.
Why Winter Is a Smart Time to Choose Regenerative Medicine
Regenerative therapies work by supporting the body’s natural ability to repair and restore damaged tissues. During the winter, this approach can be particularly beneficial for several reasons.
1. Winter Often Marks a Natural Slowdown—Perfect for Recovery
Many people slow their routines during the colder months. This makes it easier to schedule the brief downtime required after regenerative injections.
2. Reduced Activity Helps Regeneration Work Better
After treatments like PRP, patients need a window of lower impact activity. Winter’s pace naturally aligns with this healing phase.
3. Get Ahead of Spring Activity
Whether you’re preparing for gardening, sports, travel, or outdoor activities, winter treatment gives your joints time to heal so you can be more active (and pain-free) when spring arrives.
4. Regenerative Medicine Addresses the Root Cause
Unlike medications that only mask pain, regenerative therapies aim to:
- reduce inflammation
- improve blood flow
- support tissue repair
- slow or reverse degenerative processes
This makes it an ideal option for chronic winter flares.
5. Less Reliance on Seasonal Pain Medications
Patients often notice increased medication use during colder months. Regenerative care can help reduce dependence on pills or repetitive steroid injections.
Common Joint Issues Treated with Regenerative Therapy in Winter
Winter pain tends to flare in:
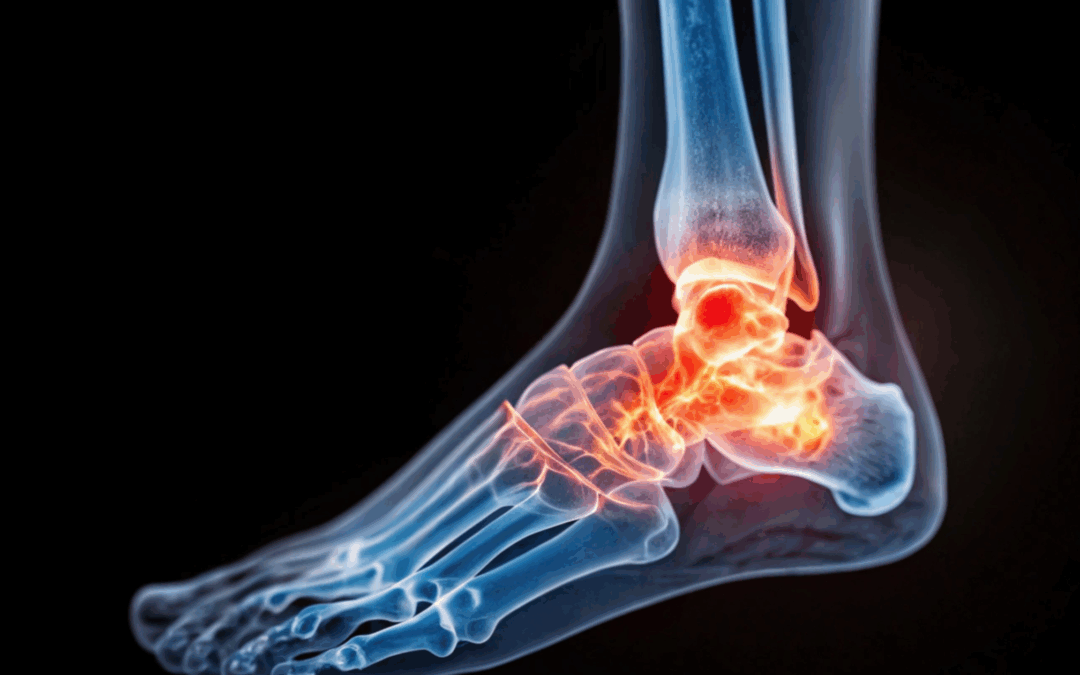
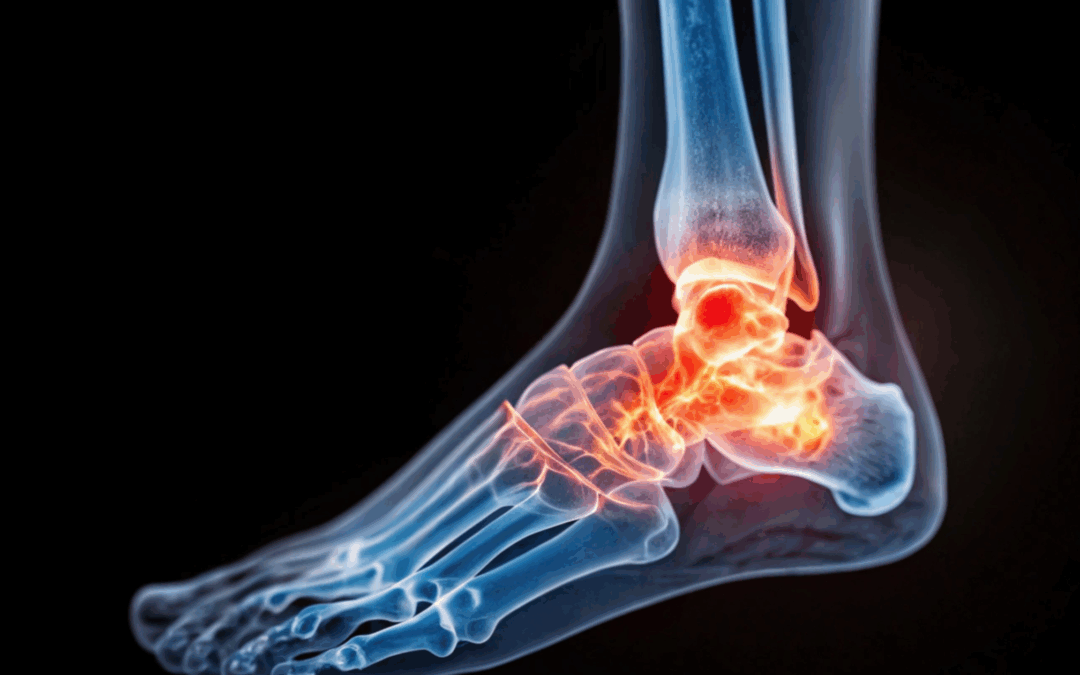
- knees (arthritis, meniscus issues, cartilage loss)
- hips (labral tears, early arthritis)
- shoulders (rotator cuff injuries, tendonitis)
- elbows (tendon degeneration)
- ankles and feet (Achilles issues, plantar fasciitis)
- spine joints (facet arthritis)
Regenerative medicine helps stabilize and strengthen these areas while reducing pain.
Types of Regenerative Treatments That Work Well in Winter
PRP Injections (Platelet-Rich Plasma)
Uses your own platelets to decrease inflammation and stimulate tissue repair.
Orthobiologics
Includes growth-factor-rich injections, micro-fat grafting, and other biologic agents that support healing.
Cell-Based Therapies
Derived from bone marrow or fat tissue to promote repair in more advanced degeneration.
Your provider will recommend options based on imaging, severity, and your activity goals.
Supporting Joint Care Through the Cold Season
Regenerative medicine works best when paired with targeted lifestyle strategies. Consider adding:
- winter-appropriate movement (indoor walking, stretching, low-impact exercise)
- anti-inflammatory nutrition
- joint-warming routines (heat therapy, warm showers before activity)
- physical therapy for mobility and strength
- proper winter footwear and traction
These habits help maintain the benefits of regenerative treatment and keep winter symptoms under control.
Is Regenerative Medicine Right for You This Winter?
If cold weather consistently makes your joint pain worse—or if you’re tired of managing symptoms year after year—this may be the perfect time to explore regenerative options. These treatments are especially helpful if:
- conservative therapies have stopped working
- pain interferes with winter activity
- you want a longer-term, non-surgical approach
- you prefer natural healing over medications
- you want to prepare your body for an active spring
Winter doesn’t have to be painful. With the right regenerative plan, you can stay mobile, reduce inflammation, and give your joints the healing support they need.
Oct 17, 2025
Joint pain often starts subtly — a little stiffness in the knees, soreness in the shoulders, or discomfort after activity. These are often signs of early joint degeneration, when cartilage and surrounding tissues begin to wear down. Fortunately, regenerative medicine offers new hope for restoring joint health before these early issues turn into chronic pain or arthritis.
Understanding Early Joint Problems
Our joints are built to move smoothly, cushioned by cartilage, lubricated by joint fluid, and supported by strong ligaments and tendons. Over time, however, wear and tear, injury, or inflammation can damage these structures.
Early joint problems may include:
- Mild stiffness or aching after activity
- Pain when bending or climbing stairs
- Swelling or tenderness around the joint
- Decreased flexibility or “creaking” sensations
At this early stage, the joint still has the potential to heal — especially with regenerative treatments that help the body repair and rebuild healthy tissue.
How Regenerative Medicine Works
Regenerative medicine focuses on stimulating the body’s natural healing processes. Rather than just masking symptoms with medication or injections, regenerative therapies aim to restore tissue health, reduce inflammation, and improve joint function.
These treatments use the body’s own biological materials — like platelets or stem cells — to encourage tissue repair and regeneration where it’s needed most.
Common Regenerative Treatments for Early Joint Damage
1. Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves concentrating platelets from your own blood and injecting them into the affected joint. These platelets contain powerful growth factors that:
- Stimulate tissue repair
- Reduce inflammation
- Promote collagen and cartilage regeneration
PRP can be used for early joint problems in the knees, shoulders, hips, or other joints — helping restore comfort and mobility naturally.
2. Stem Cell Therapy
Stem cell therapy introduces healing cells — usually derived from bone marrow or adipose (fat) tissue — into the damaged joint. These cells can help rebuild cartilage, improve cushioning, and restore balance within the joint environment.
Early research suggests stem cell therapy may slow or even reverse early degenerative joint changes, helping patients avoid or delay more invasive procedures like joint replacement.
3. Prolotherapy
Prolotherapy uses a natural dextrose-based solution injected around weakened ligaments and tendons to trigger the body’s repair response. This mild inflammation promotes the growth of stronger connective tissue, improving joint stability and function.
Over time, this can reduce pain caused by instability or early joint wear.
Benefits of Early Regenerative Intervention
Addressing joint problems early can prevent more serious degeneration and preserve mobility. The benefits of regenerative therapies include:
- Minimally invasive procedures with little to no downtime
- Reduced need for pain medications or steroids
- Improved joint strength and flexibility
- Potential long-term relief by promoting true healing rather than masking symptoms
Is Regenerative Treatment Right for You?
Regenerative therapies may be ideal if you’re experiencing mild to moderate joint pain, early arthritis, or mobility issues that haven’t improved with rest, physical therapy, or standard treatments.
A pain management or orthopedic specialist can evaluate your condition through imaging and examination to determine whether PRP, stem cell therapy, or prolotherapy is the right approach for your needs.
A Future-Focused Approach to Joint Care
Regenerative treatments are changing how we approach joint pain — emphasizing healing, repair, and long-term joint preservation. For those with early joint problems, these therapies offer a proactive, restorative way to protect joint health and maintain an active lifestyle.
If you’ve noticed stiffness or joint discomfort, now is the time to explore regenerative options. Early action can make all the difference in keeping your joints healthy and pain-free for years to come.

Jun 13, 2025
Joint pain is one of the most common and debilitating health concerns affecting millions worldwide. Whether it stems from osteoarthritis, injury, or chronic overuse, the damage to cartilage and connective tissues can significantly reduce mobility and quality of life. In recent years, cellular therapy has emerged as a promising alternative to conventional treatments like medications, steroid injections, and even surgery. But how does it work, and does the science back the hype? Let’s dive into the mechanisms, evidence, and potential of cellular therapy to repair damaged joints.
What is Cellular Therapy?
Cellular therapy, often referred to as regenerative medicine, involves using a patient’s own cells to repair or regenerate damaged tissues. In the context of joint repair, the most common types of cellular therapy include:
-
Stem cell therapy: Typically using mesenchymal stem cells (MSCs) derived from bone marrow, adipose tissue, or umbilical cords.
-
Platelet-rich plasma (PRP): A concentrate of platelets derived from the patient’s own blood, rich in growth factors that stimulate healing.
The Science Behind Joint Damage
To understand how cellular therapy might work, it’s helpful to know what happens when joints are damaged. Healthy joints are cushioned by cartilage, a smooth and slippery tissue that enables frictionless movement. However, cartilage has a limited ability to heal because it lacks a blood supply. When it wears down due to injury or disease, the body struggles to regenerate the lost tissue.
This leads to symptoms like:
Traditional treatments typically aim to manage symptoms rather than repair tissue. This is where cellular therapy seeks to make a game-changing impact—by stimulating the body to heal itself.
How Cellular Therapy Works
1. Stem Cell Therapy
Mesenchymal stem cells (MSCs) are multipotent, meaning they can differentiate into various cell types, including chondrocytes, the cells responsible for producing cartilage. When injected into the joint, these stem cells are believed to:
-
Reduce inflammation
-
Stimulate the repair of cartilage
-
Recruit other healing cells to the area
-
Modulate immune responses
Moreover, stem cells secrete bioactive molecules (cytokines and growth factors) that contribute to the repair environment. It’s not just about replacing cells—it’s about kick-starting the body’s healing process.
2. Platelet-Rich Plasma (PRP)
PRP therapy involves drawing a patient’s blood, centrifuging it to concentrate the platelets, and injecting it into the injured joint. Platelets are a natural source of growth factors, including:
-
Platelet-derived growth factor (PDGF)
-
Transforming growth factor-beta (TGF-β)
-
Vascular endothelial growth factor (VEGF)
These molecules can stimulate tissue repair, reduce inflammation, and improve pain. While PRP doesn’t contain stem cells, it can enhance the microenvironment to support natural regeneration.
What Does the Research Say?
Stem Cells: Promising but Preliminary
Numerous animal and early human studies have shown that stem cell injections can:
A 2020 meta-analysis published in The American Journal of Sports Medicine found that patients receiving MSC therapy for knee osteoarthritis showed significant improvements in pain and function compared to controls. However, these benefits vary based on factors like cell source, dosage, and disease severity.
Still, it’s important to note that most studies are small and short-term. Large-scale, randomized controlled trials (RCTs) are still needed to validate the long-term safety and effectiveness of stem cell therapy.
PRP: Growing Clinical Support
PRP has a more robust clinical foundation, particularly in treating mild to moderate osteoarthritis. Studies have shown that PRP is more effective than hyaluronic acid injections (another common joint treatment) in reducing pain and improving joint function.
In 2021, the Journal of Orthopaedic Research published a study indicating that PRP was effective in reducing knee pain for up to 12 months in osteoarthritis patients. While results are modest, PRP is considered relatively low-risk and widely used by sports medicine physicians.
Risks and Limitations
While cellular therapy holds enormous promise, it’s not without risks or limitations:
-
Lack of standardization: There is no universal protocol for dosage, preparation, or delivery.
-
Variable outcomes: Some patients experience dramatic improvement, while others see little to no benefit.
-
Regulatory status: The FDA tightly regulates stem cell therapies, and many offerings at clinics are not approved or lack scientific validation.
-
Cost: These treatments are often expensive and not covered by insurance.
Patients should exercise caution and consult with a specialist experienced in regenerative medicine before undergoing any procedure.
The Future of Cellular Therapy
Research is advancing rapidly, and future developments may include:
-
Gene-edited stem cells that are more effective at cartilage regeneration
-
Personalized medicine approaches using a patient’s unique cellular profile
-
Combined therapies, such as PRP with stem cells or scaffolds that support new tissue growth
Clinical trials are ongoing, and within the next decade, cellular therapies may become a routine part of managing joint degeneration, potentially delaying or even eliminating the need for joint replacement surgery.
Conclusion: Hype or Hope?
Cellular therapy is not a miracle cure, but it does represent a hopeful shift toward treating the root cause of joint pain rather than just the symptoms. The science is encouraging—especially for PRP and stem cell therapies—but we are still in the early stages of understanding who benefits most, how treatments should be delivered, and what long-term outcomes will look like.
For those suffering from joint pain and exploring alternatives to surgery, cellular therapy may offer a science-backed, minimally invasive option worth discussing with a medical professional. As research continues, we’re likely to see cellular therapy play an increasingly important role in the future of orthopedic and sports medicine.

Apr 14, 2025
Joint pain can be a daily struggle, affecting everything from simple walks to sleep and overall quality of life. For many, traditional treatments like physical therapy, medications, or even surgery provide only limited relief—or come with side effects and long recovery times. That’s where regenerative medicine steps in, offering innovative options like Platelet-Rich Plasma (PRP) and Cell Therapy. These treatments harness the body’s own healing powers to target the root of joint pain, not just mask the symptoms.
If you’re curious about how PRP and Cell Therapy work, and whether they might be right for you or someone you love, read on. We’ll break down the science in simple terms and explore how these therapies are changing the way we treat joint issues.
What Causes Joint Pain?
Joint pain can stem from many sources: injury, overuse, inflammation, arthritis (especially osteoarthritis), or even simple aging. The cartilage that cushions joints can wear down, tendons and ligaments can become inflamed or torn, and the surrounding tissues may degenerate over time.
Traditionally, options like corticosteroid injections or anti-inflammatory drugs have been used to reduce pain. However, these don’t actually repair damage—they just offer temporary relief. That’s where regenerative therapies like PRP and cell therapy stand apart: they aim to stimulate healing, not just dull the pain.
What Is PRP Therapy?
Platelet-Rich Plasma (PRP) therapy is a treatment that uses a concentration of your own platelets to accelerate healing in damaged joints and tissues.
How It Works:
- Blood Draw: A small amount of your blood is drawn—similar to a standard lab test.
- Separation: The blood is spun in a centrifuge to separate the platelets from other components like red and white blood cells.
- Injection: The resulting platelet-rich plasma is injected directly into the affected joint.
Platelets are best known for clotting blood, but they also contain growth factors—powerful proteins that promote tissue repair, reduce inflammation, and stimulate cell regeneration. By injecting a high concentration of these growth factors directly into the joint, PRP therapy encourages the body to repair itself.
What It’s Used For:
- Osteoarthritis (knee, hip, shoulder)
- Tendonitis
- Ligament injuries
- Cartilage damage
- Sports injuries
What Is Cell Therapy?
Cell therapy—often referred to as stem cell therapy—uses the body’s own cells to rebuild and repair damaged tissues. These aren’t embryonic stem cells but rather adult stem cells, typically derived from bone marrow or adipose (fat) tissue.
How It Works:
- Harvesting Cells: Cells are collected from your own body, usually from the bone marrow in your pelvis or fat tissue in the abdomen or thighs.
- Processing: The cells are processed and sometimes combined with PRP to enhance their effectiveness.
- Injection: The mixture is injected into the painful joint under ultrasound or fluoroscopic guidance.
These cells have the ability to differentiate—meaning they can transform into other types of cells, such as cartilage, bone, or tendon cells. They also release molecules that reduce inflammation and promote healing at the cellular level.
What It’s Used For:
- Moderate to severe osteoarthritis
- Cartilage degeneration
- Chronic joint inflammation
- Joint injuries that haven’t healed with traditional treatments
PRP vs. Cell Therapy: What’s the Difference?
| Feature |
PRP Therapy |
Cell Therapy |
| Source |
Platelets from your blood |
Stem cells from bone marrow or fat |
| Mechanism |
Stimulates healing with growth factors |
Repairs tissue by regenerating new cells |
| Best For |
Mild to moderate joint damage |
Moderate to severe degeneration |
| Invasiveness |
Minimally invasive |
Slightly more invasive (requires tissue harvesting) |
| Cost |
Lower |
Higher |
Think of PRP as a “booster” that speeds up healing, while cell therapy is a “builder” that can regenerate more extensive damage.
What to Expect from Treatment
Procedure:
Both PRP and cell therapy are usually done in an outpatient setting. The procedures typically take 1-2 hours. Since your own cells are used, the risk of allergic reactions is minimal.
Recovery:
- PRP: Mild soreness for a day or two; most people resume normal activity within 24-48 hours.
- Cell Therapy: Slightly longer recovery time due to the harvesting process; some patients may need a few days of rest.
Results:
- Most patients report a gradual reduction in pain over weeks to months.
- Improvements can last anywhere from 6 months to 2 years or more.
- Outcomes vary depending on the severity of the condition, overall health, and adherence to post-treatment guidelines like physical therapy and lifestyle changes.
The Science Behind It
PRP and cell therapy are backed by a growing body of research. For example:
- A 2020 study published in American Journal of Sports Medicine found that PRP injections significantly improved symptoms in patients with knee osteoarthritis over a 12-month period.
- A 2021 meta-analysis concluded that stem cell therapy showed consistent results in improving joint function and reducing pain in osteoarthritis patients, especially when used early in disease progression.
While not a miracle cure, these therapies are helping people delay or even avoid surgery, including joint replacement.
Is It Safe?
Yes—for most patients, PRP and cell therapy are considered safe and well-tolerated. Because the materials come from your own body, the risk of infection or rejection is extremely low. However, like any medical procedure, results aren’t guaranteed, and not everyone is a good candidate.
It’s crucial to consult with a medical provider who specializes in regenerative medicine to determine if these treatments are appropriate for your condition.
Is It Covered by Insurance?
Unfortunately, most insurance companies don’t yet cover PRP or cell therapy, viewing them as experimental. That’s slowly changing as more evidence emerges. Costs can range from a few hundred dollars (for PRP) to several thousand (for cell therapy), so be sure to ask for a cost estimate before committing.
Who’s a Good Candidate?
You might be a good candidate for PRP or cell therapy if you:
- Have chronic joint pain that hasn’t improved with rest, therapy, or medication
- Want to avoid or delay surgery
- Are in good general health
- Are not a smoker (smoking reduces healing)
- Are not severely immunocompromised or on blood thinners
The Future of Joint Pain Treatment
PRP and cell therapy offer a promising new frontier in the treatment of joint pain. These regenerative therapies don’t just cover up symptoms—they tap into the body’s natural ability to heal, rebuild, and regenerate. While they’re not a replacement for all conventional treatments, they can be a powerful tool in the journey to pain relief, better mobility, and improved quality of life.
If joint pain is holding you back, it may be time to consider a regenerative approach. Consult a knowledgeable provider to explore whether PRP or cell therapy is the right path for you.
Disclaimer: This article is for informational purposes only and should not be taken as medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment recommendations.

Oct 13, 2022
As one the largest joints in the body, the knees often suffer the most from the wear-and-tear that comes with a lifetime of use (or abuse). Whether damaged by an injury such as a ligament or tendon tear, or simply worn down by years of standing, running, jumping, lifting, etc., the result is often the same: chronic pain, inflammation, and reduced movement.
Depending on the extent of the injury or damage to the knee, patients can often gain some temporary relief from steroid injections that decrease swelling or from other interventional treatments such as hyaluronic acid injections that increase lubrication in the joint. But when these options have been expended, many look to surgery as their last, best hope to repair the damage and bring sought-after pain relief.
But now, non-surgical cellular treatments are providing long-term relief to patients with knee pain by putting the body’s own natural healing abilities to work to undo the damage brought on by injury or degeneration.
How Do Cellular Treatments Work?
Known as regenerative medicine, cellular treatments harness powerful healing properties within the body’s building blocks—its own cells—to help repair and, in some cases, replace injured tissues. These treatments promote healing of injuries to the cartilage in the knee joint, as well as soft tissues such as tendons and ligaments in the knee.
To adhere to Federal Food and Drug Administration (FDA) guidelines, only autologous (from the patient’s own body) cellular products can be used to treat orthopedic conditions. Donor products, including cord or amniotic cells, are not approved to treat knee osteoarthritis or soft tissue injuries in the knee.
Cellular products are taken from the patient’s own blood, bone marrow, or fat (adipose) tissues to maximize the benefits of their unique healing properties:
- Platelet Rich Plasma: Platelets in blood release growth factors and proteins that promote tissue repair, while the plasma carries the hormones, electrolytes and nutrients required to nourish cells during the healing process. Platelet rich plasma treatments can be customized to create specific formulations for each type of tissue being treated (muscle, tendon, ligament, cartilage).
- Cellular Therapy: Cells derived from the patient’s own bone marrow or adipose (fat) tissue called “pericytes” produce molecules that spur the production of new blood vessels, awaken other stem cells and encourage newly forming cells to produce collagen and other proteins essential for creating new healthy tissues. These specific cells can develop into the specific kind of cell needed, whether that be tendon, ligament, cartilage, or bone.
After these products are removed from the patient, they are concentrated and reinjected directly to the injured area to address the degeneration or injury.
Do Cellular Treatments for the Knees Work?
Regenerative medicine practitioners have scores of anecdotal evidence from satisfied patients that support the powerful pain-relieving and healing properties of cellular treatments for the knees.
But because the field of regenerative medicine is relatively new, until recently, there has been a limited amount of clinical data to bolster this anecdotal evidence. We believe the quantitative, controlled data that clinical trials will produce will not only further the use of cellular treatments for orthopedic conditions but will also confirm what hundreds of our satisfied patients have been telling us for years: cellular treatments have helped their bodies heal naturally while allowing them to resume the activities that help them regain their quality of life.
The experts at SDOMG help patients with knee injuries and knee osteoarthritis find the relief they need using expert technology and treatments. To learn more about cellular therapy for knee injuries, contact SDOMG using the form below.