Dec 12, 2025
Joint degeneration doesn’t happen overnight. It’s a slow, progressive process — but the earliest warning signs are often subtle enough that many people shrug them off as “getting older” or “overdoing it.” Identifying these changes early can make all the difference in treatment outcomes, mobility, and long-term joint health. And thanks to advances in regenerative medicine, patients now have powerful options that can protect, repair, and even restore damaged tissue before the problem becomes severe.
Below, we break down the early symptoms to watch for and explore how modern regenerative therapies can help interrupt the degenerative cascade.
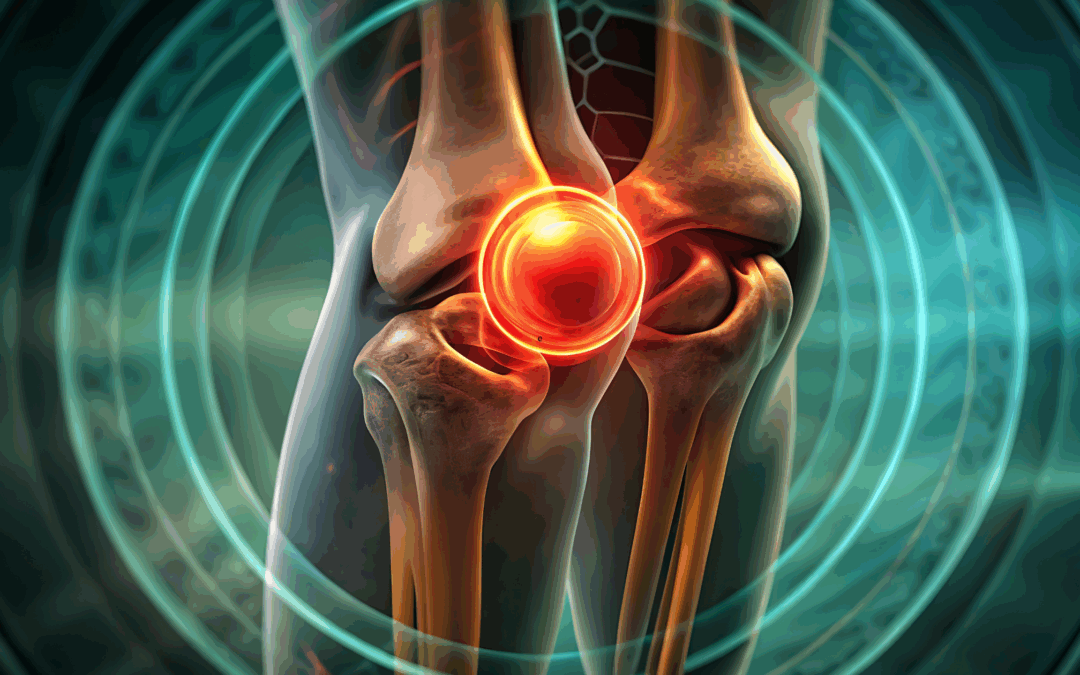
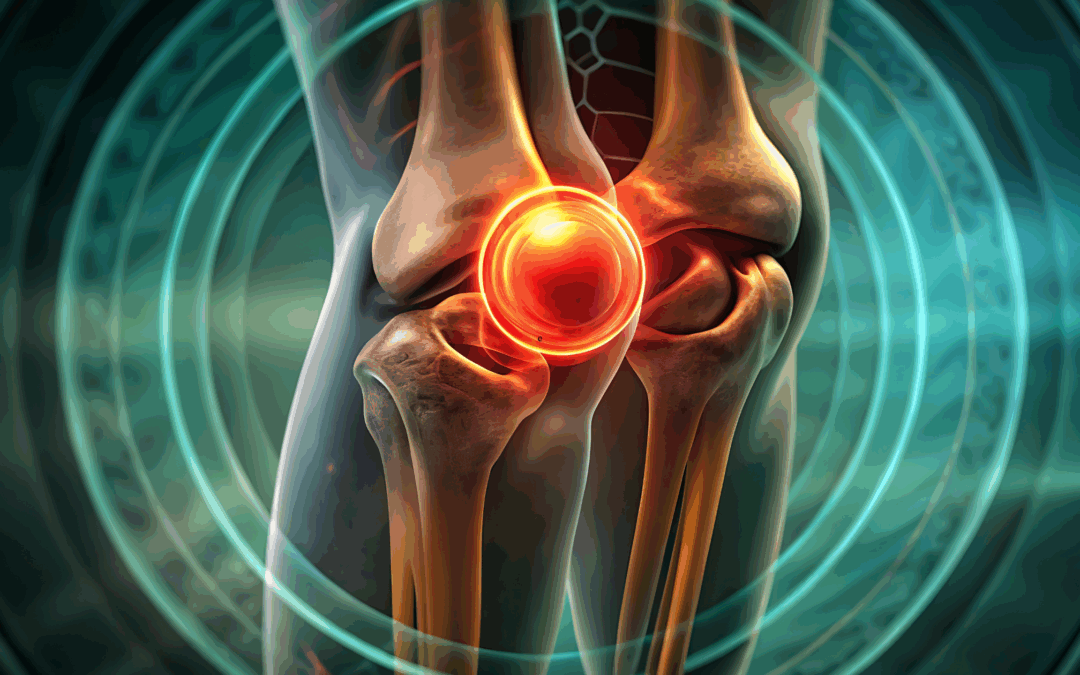
What Early Joint Degeneration Looks Like
1. Persistent Morning Stiffness
If you feel “rusty” or tight first thing in the morning — especially in the knees, hips, or spine — this can indicate early cartilage wear or inflammation. Stiffness that improves as you move around is a classic hallmark of early degenerative changes.
2. Clicking, Popping, or Grinding
Noisy joints aren’t always dangerous, but when those sounds are paired with discomfort, swelling, or instability, they may signal roughened surfaces or early cartilage breakdown.
3. Pain With Activity That Improves With Rest
You might feel fine at rest but experience dull aching during:
- Walking up or down stairs
- Long periods of standing
- Squatting or lifting
- High-impact workouts
This “use-related pain” often shows up years before advanced arthritis.
4. Swelling or Warmth Around the Joint
Mild inflammation is one of the earliest internal reactions to joint stress or degeneration. Even occasional swelling after activity can indicate chronic irritation inside the joint.
5. Reduced Range of Motion
Maybe your knee doesn’t bend the way it used to, or your shoulder feels tight when reaching overhead. Loss of flexibility is often one of the first measurable signs of joint deterioration.
6. Fatigue or Weakness in the Joint
Muscles surrounding a degenerating joint often work overtime to compensate, which can create fatigue, shakiness, or weakness during routine tasks.
Why Early Action Matters
Once cartilage has worn away significantly, it cannot regenerate on its own — and late-stage arthritis often requires aggressive treatments like joint replacement. Early intervention, however, can slow or even stop the degenerative cycle. The goal is to reduce inflammation, restore stability, and stimulate natural repair pathways before more permanent damage occurs.
This is where regenerative medicine shines.
How Regenerative Therapies Can Help
Platelet-Rich Plasma (PRP)
PRP concentrates your body’s own growth factors to:
- Reduce inflammation
- Promote tissue repair
- Slow cartilage breakdown
- Improve joint lubrication
Great for early osteoarthritis, tendon irritation, and chronic joint strain.
Orthobiologics
These treatments use biologically active cells and proteins to enhance healing in damaged tissue. Orthobiologics can improve structural stability, reduce inflammation, and support long-term joint health.
Cell–Based Therapies
These therapies may help stimulate new tissue formation in joints that show early degenerative changes. They can support:
- Cartilage protection
- Improved mobility
- Reduced pain
- Enhanced shock absorption
Especially useful for knees, hips, shoulders, and spine-related degeneration.
Hyaluronic Acid (Viscosupplementation)
A lubrication-boosting gel injected into the joint to:
- Improve glide
- Reduce pain
- Support smoother movement
Works well for mild to moderate osteoarthritis.
Lifestyle + Regenerative = Long-Term Prevention
The best outcomes happen when regenerative therapies are paired with:
- Strength training
- Weight management
- Physical therapy
- Anti-inflammatory nutrition
- Activity modification
Together, these strategies help reinforce joint support structures and reduce ongoing stress.
When to Seek Evaluation
You don’t need severe pain to justify seeing a specialist. In fact, the sooner you understand what’s happening inside your joints, the more options you have to preserve their health.
Seek evaluation if you notice:
- Recurring stiffness
- Activity-related pain
- Early swelling
- Clicking or grinding
- Weakness or instability
A simple exam — sometimes paired with X-ray or ultrasound — can determine your level of joint degeneration and whether regenerative therapies are appropriate.
Final Thoughts
Joint degeneration doesn’t have to be inevitable or irreversible — especially when it’s caught early. Modern regenerative options offer patients a chance to protect and restore joint health naturally, often delaying or avoiding more invasive procedures down the line.
If you’re starting to notice the early signs, now is the perfect time to explore your options and take proactive steps to keep your joints strong, mobile, and pain-free for years to come.
Aug 15, 2025
Living with chronic pain can feel like you’re constantly walking a fine line. On one side, staying active helps manage pain and maintain mobility; on the other, pushing too hard can lead to flare-ups and setbacks. The good news? You don’t need to run marathons, lift heavy weights, or endure high-impact workouts to reap the benefits of physical activity. Safe, low-impact exercises can help you stay active, improve strength, and enhance your overall quality of life—without overloading your joints or triggering unnecessary pain.
In this guide, we’ll explore why movement is essential for managing chronic pain, the types of exercises that are safest, and practical tips to make exercise a sustainable part of your routine.
Why Exercise Matters When You Have Chronic Pain
When your body hurts, it’s natural to want to move less. But inactivity often creates a vicious cycle: muscles weaken, joints stiffen, and your pain threshold can actually decrease over time. Regular, gentle movement offers multiple benefits:
- Improves circulation – helping to deliver oxygen and nutrients to muscles and tissues.
- Maintains joint flexibility – preventing stiffness that can worsen discomfort.
- Strengthens muscles – which helps support and protect painful areas.
- Boosts mood – releasing endorphins, your body’s natural pain relievers.
- Reduces inflammation – through consistent, moderate physical activity.
The key is to choose activities that work with your body, not against it.
Principles of Safe Exercise for Chronic Pain
Before jumping into specific exercise options, keep these guiding principles in mind:
- Start Slow, Progress Gradually – Overdoing it on day one can lead to flare-ups. Build up your time and intensity over weeks, not days.
- Listen to Your Body – Discomfort is normal when starting something new, but sharp or worsening pain is a red flag.
- Prioritize Consistency Over Intensity – A few minutes of movement daily is often more effective than occasional intense sessions.
- Incorporate Rest and Recovery – Your muscles and joints need time to adapt.
- Work With a Professional – A physical therapist or certified trainer with experience in chronic pain can help create a safe, tailored plan.
Low-Impact Exercises to Try
1. Walking
Walking is one of the simplest, most accessible exercises for chronic pain. It’s weight-bearing, which helps keep bones strong, yet gentle enough for most people. Start with short, 5–10 minute walks, and gradually increase your duration.
Pro tip: Invest in supportive shoes and consider walking on softer surfaces like grass or a track to reduce joint stress.
2. Swimming & Water Aerobics
Water provides buoyancy, which takes pressure off joints while still offering gentle resistance for muscle strengthening. Swimming laps, doing water aerobics, or even walking in the shallow end can improve cardiovascular health and mobility.
Bonus: Warm pools can help relax tight muscles and soothe soreness.
3. Cycling
Stationary or outdoor cycling is low-impact yet effective for building leg strength and improving endurance. A recumbent bike is often more comfortable for those with back or hip pain because it offers extra support.
4. Gentle Yoga
Yoga focuses on flexibility, balance, and controlled breathing—helpful for both physical and mental aspects of chronic pain. Look for gentle or restorative yoga classes, and avoid positions that cause sharp discomfort.
Tip: Inform your instructor about your condition so they can offer modifications.
5. Pilates
Pilates strengthens the core muscles, which play a big role in supporting the spine and reducing pain. Choose a beginner or therapeutic class and use props like resistance bands or small balls for extra support.
6. Tai Chi
This ancient martial art uses slow, flowing movements and deep breathing. It’s been shown to improve balance, coordination, and pain management, particularly in people with arthritis and fibromyalgia.
7. Resistance Band Training
Light resistance bands allow you to strengthen muscles without heavy weights. They’re gentle on joints and can be adapted to your fitness level. Exercises like seated rows, bicep curls, and leg presses can be performed slowly and mindfully.
8. Stretching Routines
Daily stretching keeps muscles limber and helps reduce stiffness. Focus on major muscle groups and move through each stretch gently, avoiding any bouncing or jerking motions.
Sample Weekly Low-Impact Activity Plan
| Day |
Activity |
Duration |
| Monday |
Gentle Yoga |
20 mins |
| Tuesday |
Walking |
15–30 mins |
| Wednesday |
Water Aerobics |
30 mins |
| Thursday |
Pilates |
20 mins |
| Friday |
Walking or Stationary Cycling |
20 mins |
| Saturday |
Tai Chi |
20 mins |
| Sunday |
Stretching |
10–15 mins |
Tips for Making Exercise Easier and More Enjoyable
- Use Heat Before Activity – Applying a heating pad or taking a warm shower before exercise can loosen stiff joints and muscles.
- Stay Hydrated – Proper hydration supports muscle function and helps prevent cramping.
- Break It Into Small Chunks – Two 10-minute sessions can be just as beneficial as one 20-minute workout.
- Track Your Progress – Keep a journal of your activities and how you feel afterward to identify patterns.
- Find a Buddy – Exercising with a friend provides motivation and accountability.
When to Stop and Seek Help
Mild soreness after starting a new activity is normal, but you should stop exercising and consult a healthcare professional if you experience:
- Sharp, stabbing, or severe pain
- Significant swelling
- Dizziness or shortness of breath
- Pain that persists or worsens over several days
The Bottom Line
Living with chronic pain doesn’t mean giving up on an active lifestyle—it just means adapting it. Low-impact exercises like walking, swimming, yoga, and tai chi can help you stay mobile, strengthen muscles, and improve your mental well-being without pushing your body into painful territory.
By starting slowly, choosing activities you enjoy, and listening to your body, you can make movement a powerful ally in managing chronic pain for the long term.

Apr 23, 2025
Arthritis affects over 58 million adults in the United States alone, making it a leading cause of disability and pain. Traditionally, treatment options have focused on symptom management through medications, physical therapy, and, in severe cases, joint replacement surgery. However, recent advances in regenerative medicine are changing the landscape of arthritis care by offering promising, non-surgical alternatives that aim to repair and restore damaged tissues.
In this post, we’ll explore the latest regenerative medicine techniques used to treat arthritis, how they work, and why they’re generating excitement among physicians and patients alike.
Understanding Arthritis and Its Impact
Arthritis is not a single disease but a term that covers more than 100 different types of joint conditions. The most common forms are osteoarthritis (OA) and rheumatoid arthritis (RA):
- Osteoarthritis is a degenerative joint disease where the cartilage that cushions bones wears down over time.
- Rheumatoid arthritis is an autoimmune condition where the immune system attacks the synovial lining of the joints, causing inflammation and tissue damage.
Regardless of the type, arthritis often leads to joint pain, stiffness, decreased mobility, and a diminished quality of life.
Why Patients Seek Non-Surgical Options
Joint replacement surgery, while effective, comes with risks: infection, blood clots, lengthy recovery periods, and even the potential for implant failure over time. Many patients are not ready—or suitable candidates—for surgery and seek less invasive options to manage symptoms and improve joint function.
That’s where regenerative medicine steps in.
What Is Regenerative Medicine?
Regenerative medicine harnesses the body’s natural healing mechanisms to repair or replace damaged tissues, including cartilage, ligaments, tendons, and even bone. These treatments aim to not only reduce symptoms but also to slow or potentially reverse the progression of arthritis.
The most promising regenerative therapies for arthritis include:
- Platelet-Rich Plasma (PRP) Therapy
- Cell-Based Therapy
- Prolotherapy
Let’s break down each of these innovative techniques.
-
Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves drawing a small amount of the patient’s blood, processing it to concentrate the platelets, and then injecting this platelet-rich plasma into the affected joint.
How It Works:
Platelets contain growth factors that help stimulate tissue regeneration and reduce inflammation. When injected into an arthritic joint, PRP can:
- Promote cartilage healing
- Decrease pain and stiffness
- Improve joint function
Clinical Evidence:
Studies have shown PRP can be more effective than corticosteroids or hyaluronic acid injections in relieving knee osteoarthritis symptoms. Results are typically seen within weeks and can last for several months or even over a year.
-
Cell-Based Therapy
Stem cells are undifferentiated cells capable of transforming into various tissue types, including cartilage. In arthritis treatment, mesenchymal stem cells (MSCs) are commonly harvested from a patient’s bone marrow or adipose (fat) tissue and injected into the joint.
How It Works:
Once inside the joint, stem cells can:
- Stimulate repair of damaged cartilage
- Modulate inflammation
- Recruit other cells to aid in tissue regeneration
Clinical Evidence:
Early studies have reported significant improvements in pain, mobility, and cartilage thickness following stem cell injections. While more research is needed to establish standardized protocols, the outlook is encouraging—especially for early to moderate osteoarthritis.
-
Prolotherapy
Prolotherapy is a regenerative injection technique that involves injecting a natural irritant—often a dextrose (sugar) solution—into the joint or surrounding ligaments and tendons.
How It Works:
The solution triggers a localized inflammatory response, prompting the body to send healing cells to the area. Over time, this can strengthen connective tissues and stabilize the joint.
Who It’s For:
Prolotherapy is particularly effective for patients with joint instability, ligament laxity, or early-stage arthritis. It’s less commonly used for severe osteoarthritis but can still play a role as part of a broader regenerative plan.
Benefits of Regenerative Medicine for Arthritis
- Minimally Invasive: Most procedures are outpatient and involve little to no downtime.
- Reduced Dependence on Medications: Patients may rely less on NSAIDs, opioids, or corticosteroids.
- Slowed Disease Progression: Some therapies show the potential to halt or even reverse cartilage loss.
- Improved Quality of Life: Many patients report enhanced mobility, reduced pain, and greater participation in daily activities.
Important Considerations
Not a One-Size-Fits-All Solution
Regenerative therapies work best in the early to moderate stages of arthritis. They may not be as effective for patients with advanced joint deterioration.
Costs and Coverage
These treatments are often not covered by insurance and can range from a few hundred to several thousand dollars per session. However, many patients find the cost worthwhile for the benefits they experience.
Choose a Qualified Provider
It’s essential to seek care from physicians who specialize in regenerative medicine and follow best practices for safety, preparation, and delivery. Improper technique or unregulated products can result in complications.
The Future of Arthritis Treatment
Regenerative medicine is rapidly evolving. As research deepens and technology advances, these therapies may soon become mainstream components of arthritis care. Clinical trials are underway to determine long-term outcomes, best candidates, and optimal treatment protocols.
What’s exciting is that these approaches shift the paradigm from merely managing symptoms to actively promoting healing—a revolutionary step for the millions living with arthritis.
Final Thoughts
If you’re struggling with arthritis pain and looking for alternatives to surgery, regenerative medicine offers a promising path forward. From PRP to stem cells and beyond, these innovative techniques can help restore joint health, improve function, and reduce your reliance on medications.
Always consult a qualified healthcare professional to determine which therapy, if any, is right for you. With the right approach, living well with arthritis is not only possible—it’s becoming increasingly probable.
Interested in learning more about regenerative treatments? Talk to a regenerative medicine specialist or rheumatologist to explore your options based on your specific type of arthritis and stage of progression.

Feb 28, 2025
In recent years, medical science has made significant advancements in regenerative medicine, one of which is Lipogems. This innovative technique utilizes adipose (fat) tissue to harness the body’s natural healing properties. Lipogems stands out as a minimally invasive procedure that offers promising results for patients suffering from various musculoskeletal conditions. By employing the unique characteristics of adipose-derived stem cells, it aims to reduce inflammation and promote tissue repair.
The essence of Lipogems lies in its ability to extract and process adipose tissue, which is abundant in stem cells and growth factors. This procedure not only provides a source of regenerative cells but also offers a scaffold for tissue healing. As a result, it has garnered attention in the fields of orthopedics, sports medicine, and aesthetic treatments, making it a versatile option for many patients.
As more individuals seek alternatives to traditional surgical methods, the demand for therapies like Lipogems continues to rise. This article aims to delve into the science behind Lipogems, its procedural aspects, and the conditions it effectively treats, providing a comprehensive understanding of this revolutionary healing technique.
The Science Behind Lipogems: Understanding Adipose-Derived Stem Cells
At the core of Lipogems therapy are adipose-derived stem cells (ADSCs). These cells are unique due to their ability to differentiate into various cell types, including bone, cartilage, and fat cells. This versatility makes them invaluable in regenerative medicine. Research has shown that ADSCs possess anti-inflammatory properties, which can significantly aid in the healing process.
Adipose tissue is rich in these stem cells, making it an excellent source for regenerative therapies. Unlike other sources, such as bone marrow, adipose tissue can be harvested easily and in larger quantities, providing a substantial number of stem cells for therapeutic use. Additionally, the processing of adipose tissue in Lipogems preserves the architecture and microenvironment necessary for stem cell function, enhancing their effectiveness.
Understanding the role of these stem cells is crucial for appreciating how Lipogems works. When injected into damaged tissues, ADSCs promote healing by stimulating the regeneration of damaged cells and reducing inflammation. This natural approach aligns with the body’s intrinsic healing mechanisms, offering a safer and often more effective alternative to conventional treatments.
How Lipogems Works: Step-by-Step Process
The Lipogems procedure is designed to be efficient and minimally invasive. Here’s a step-by-step overview of how it works:
- Consultation and Assessment: The process begins with a thorough consultation where the physician evaluates the patient’s medical history and current condition. This assessment helps determine if Lipogems is a suitable option for the individual.
- Harvesting Adipose Tissue: Once deemed appropriate, a small amount of adipose tissue is harvested, typically from the abdomen or thighs. This is done using liposuction, a minimally invasive technique that involves making small incisions to extract the fat.
- Processing the Tissue: The harvested adipose tissue is then processed using the Lipogems technology, which involves washing and breaking down the fat. This process isolates the stem cells and growth factors while preserving the natural extracellular matrix, which is vital for healing.
- Injection into the Target Area: After processing, the resulting solution containing stem cells and growth factors is injected into the area requiring treatment. This could be a joint, tendon, or other damaged tissue, depending on the patient’s condition.
- Post-Procedure Care: Following the injection, patients are provided with care instructions to facilitate healing. This may include rest, physical therapy, or follow-up appointments to monitor progress.
By understanding this step-by-step process, patients can appreciate the meticulous care involved in Lipogems, ensuring that they receive the best possible treatment tailored to their needs.
Conditions Treated with Lipogems Technology
Lipogems technology has shown efficacy in treating a variety of conditions. Here are some of the most common applications:
- Osteoarthritis: This degenerative joint disease often results in significant pain and reduced mobility. Lipogems can help by restoring joint function and alleviating discomfort through its regenerative effects.
- Tendinopathies: Conditions such as tennis elbow and Achilles tendonitis can benefit from Lipogems injections. The stem cells work to repair damaged tissues, promoting healing and reducing pain.
- Cartilage Damage: Injuries to cartilage can lead to long-term complications. Lipogems provides a source of cells that can regenerate cartilage, potentially delaying or avoiding joint replacement surgery.
- Sports Injuries: Athletes frequently face injuries that require quick and effective treatment. Lipogems has emerged as a promising option for treating soft tissue injuries, allowing athletes to return to their sport sooner.
- Aesthetic Applications: Beyond orthopedic uses, Lipogems can also be utilized in cosmetic procedures, such as facial rejuvenation, where regenerative properties can improve skin texture and volume.
The versatility of Lipogems makes it an attractive option for a range of conditions, allowing patients to explore alternatives to traditional treatment methodologies.
The Lipogems Procedure: What to Expect
Patients considering Lipogems can expect a well-structured procedure that prioritizes comfort and safety. Here’s what to anticipate during the entire process:
- Preparation: Before the procedure, patients are advised to follow specific guidelines, such as avoiding blood thinners and alcohol. This preparation helps minimize complications and ensures a smoother experience.
- Local Anesthesia: To enhance comfort during the fat harvesting process, local anesthesia is administered. This allows the procedure to be performed with minimal discomfort, ensuring that patients remain relaxed throughout.
- Fat Harvesting and Processing: The liposuction process typically takes around 30 minutes, followed by the processing of the adipose tissue. The entire procedure, from harvesting to injection, can be completed in about one to two hours.
- Injection and Follow-Up: After processing, the injection is performed using ultrasound guidance for precision. Patients usually experience minimal downtime, with many resuming normal activities within a few days. Follow-up appointments are scheduled to monitor progress and assess the effectiveness of the treatment.
Patients can feel reassured knowing that the Lipogems procedure is designed to be efficient, with a focus on achieving optimal results while ensuring their comfort throughout the process.
Recovery and Results: Healing with Lipogems
Understanding the recovery process is vital for patients undergoing Lipogems treatment. The timeline for recovery can vary based on the individual and the condition being treated. However, most patients can expect the following:
- Initial Recovery: After the procedure, patients may experience mild swelling or discomfort in the treated area. This is typically manageable with over-the-counter pain relievers and should subside within a few days.
- Physical Activity: Patients are generally encouraged to resume light activities shortly after the procedure, while more strenuous activities may be restricted for a few weeks. Adhering to the physician’s recommendations regarding physical activity ensures optimal healing.
- Long-Term Results: Many patients begin to notice improvements in their symptoms within several weeks. However, the full benefits of Lipogems may take several months to manifest as the body continues to heal and regenerate damaged tissues.
The regenerative capabilities of Lipogems can lead to significant improvements in pain relief and mobility, with many patients reporting enhanced quality of life post-treatment.
Who is a Good Candidate for Lipogems Treatment?
Determining eligibility for Lipogems treatment involves a careful evaluation by a qualified healthcare professional. Generally, good candidates include:
- Individuals with Chronic Pain: Patients suffering from chronic joint pain, tendonitis, or injuries that have not responded to conventional treatments may benefit from Lipogems.
- Active Individuals: Those who lead an active lifestyle, including athletes, who seek quick recovery from injuries often find Lipogems to be an appealing option.
- Patients with Degenerative Conditions: Individuals with conditions like osteoarthritis or cartilage damage may find relief through Lipogems, especially if they wish to avoid surgical interventions.
However, not everyone may be suitable for this treatment. Factors such as underlying health conditions, obesity, or the presence of infections may disqualify some individuals. A thorough consultation with a healthcare provider is essential to assess suitability and discuss potential risks and benefits.
Is Lipogems Right for You?
As regenerative medicine continues to evolve, Lipogems emerges as a promising option for those seeking alternatives to traditional treatments. Its minimally invasive nature, coupled with the use of the body’s own healing mechanisms, presents patients with an opportunity for recovery without the risks associated with more invasive surgeries.
Considering the various conditions treated by Lipogems and the positive outcomes reported by many patients, it is worth exploring whether this innovative therapy aligns with their health needs. Consulting a knowledgeable healthcare provider can help individuals determine if Lipogems is the right choice for them and provide personalized insights into the potential benefits and expected results.
If you’re interested in learning more about Lipogems and how it can help you on your healing journey, reach out to a qualified physician today to explore your options.

Jan 12, 2024
Osteoarthritis is a degenerative joint disease that affects millions of people worldwide. It occurs when the protective cartilage that cushions the ends of bones wears down over time, leading to pain, swelling, and stiffness. While there is no cure for osteoarthritis, several treatment options are available to manage the symptoms and improve quality of life. In this article, we will explore the latest advancements in osteoarthritis treatments, including both surgical and non-surgical options, as well as lifestyle changes that can support the overall treatment plan.
Understanding Osteoarthritis
Before delving into the various treatment options, it is essential to understand the basics of osteoarthritis. Osteoarthritis can affect any joint in the body, including the joints in the hands, knees, hips, shoulders, and spine. As the cartilage deteriorates, the bones may start to rub against each other, causing pain and inflammation. The exact cause of osteoarthritis is still unknown, but factors such as age, genetics, and previous joint injuries can increase the risk.
Common Symptoms of Osteoarthritis
Osteoarthritis can manifest differently in each individual, but there are several common symptoms to watch out for. These include joint pain and stiffness, especially after periods of inactivity or overuse. Swelling around the affected joint may also occur, making moving or performing daily activities difficult. Sometimes, a grating sensation or the feeling of bones rubbing together can be experienced. It is crucial to consult a healthcare professional if any of these symptoms persist, as early diagnosis and treatment can help slow down the progression of the disease.
The Latest Advancements in Osteoarthritis Treatments
In recent years, significant advancements have been made in the field of osteoarthritis treatments. One such development is the use of regenerative medicine techniques, including platelet-rich plasma (PRP) therapy and other cell-based therapies. PRP therapy involves injecting a concentrated solution of the patient’s own blood platelets into the affected joint, promoting healing and reducing inflammation. Another option is utilizing a patient’s own mesenchymal stem cells from their fat or bone marrow to promote healing and repair of injured cartilage.
Additionally, researchers are exploring the potential of gene therapy in treating osteoarthritis. By targeting specific genes involved in cartilage degeneration, scientists hope to develop new therapies that can slow down or halt the progression of the disease.
Other Non-surgical Options for Managing Osteoarthritis
While surgical interventions may be necessary in severe cases of osteoarthritis, there are several non-surgical options available to manage pain and improve joint function. Physical therapy plays a crucial role in reducing pain and increasing mobility through targeted exercises and stretches.
Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen, are commonly used to alleviate osteoarthritis symptoms. However, it is essential to consult a healthcare professional before starting any medication regimen, as they can have side effects and interactions with other medications.
Lifestyle Changes to Support Osteoarthritis Treatments
In addition to medical interventions, certain lifestyle changes can greatly support the overall management of osteoarthritis. Maintaining a healthy weight is crucial, as excess weight stresses the joints, exacerbating symptoms. Regular exercise, such as low-impact activities like swimming or cycling, can help strengthen the muscles around the joints and improve joint flexibility.
Dietary modifications can also play a role in managing osteoarthritis. Including foods rich in omega-3 fatty acids, such as fatty fish and walnuts, can help reduce inflammation. Avoiding processed foods, sugary beverages, and excessive alcohol consumption can also have a positive impact on overall joint health.
Conclusion
In conclusion, while there is no cure for osteoarthritis, various treatment options are available to manage the symptoms and improve quality of life. From the latest advancements in regenerative medicine to non-surgical interventions and lifestyle changes, individuals with osteoarthritis have a range of options to explore. It is crucial to work closely with a healthcare professional to develop a personalized treatment plan that addresses each individual’s specific needs and goals. By staying informed about the latest advancements in osteoarthritis treatments, individuals can make informed decisions and take control of their joint health.
Consult a healthcare professional today at SDOMG to explore the best treatment options for osteoarthritis and take control of your joint health. Fill out the form below to learn more.

Dec 20, 2023
Cellular therapy has emerged as a groundbreaking medical treatment, revolutionizing the field of healthcare. By utilizing the body’s own cells, this innovative approach seeks to restore health and promote healing in a way that traditional medicine cannot always achieve. In this article, we will delve into the world of cellular therapy, exploring its definition, history, mechanism of action, benefits, and more.
What is Cellular Therapy?
Cellular therapy, also known as cell therapy or cytotherapy, involves transplanting living cells into a patient’s body to replace or repair damaged cells or tissues. These cells can be derived from the patient’s own body. In most circumstances, platelets or mesenchymal cells are used for this type of therapy. Platelets are the tiny cells in a patient’s blood that secrete numerous growth factors which are critical in healing. Mesenchymal cells are multipotent cells found in fat or bone marrow and have the ability to differentiate into bone, cartilage, tendon/ligament, and muscle. Cellular therapy aims to enhance the body’s natural healing processes and restore proper functioning.
History of Cellular Therapy
The history of cellular therapy can be traced back to the late 19th century when bone marrow transplantation was first attempted. This procedure involved the transfer of healthy bone marrow cells to individuals suffering from blood disorders, such as leukemia. Over the years, advancements in medical research and technology have expanded the applications of cellular therapy to various conditions, including organ transplantation, immune system disorders, neurodegenerative diseases, and orthopedics.
How It Works
Cellular therapy harnesses the power of cells to promote healing and restore health. The process begins with the collection of the desired cells, which are then prepared for transplantation. These cells are carefully administered to the patient, typically through an image guided injection targeting the affected area. Once inside the body, the cells integrate themselves into the surrounding tissues and initiate the healing process. They either replace damaged cells directly or stimulate the body’s own cells to repair and help grow new tissues, leading to improved health outcomes.
Benefits of Cellular Therapy
Cellular therapy offers numerous benefits, making it a promising treatment option for a wide range of orthopedic conditions. One significant advantage is its ability to provide personalized medicine. Since cellular therapy utilizes the patient’s own cells, the risk of rejection or adverse reactions is significantly reduced. This personalized approach also allows for targeted treatment, increasing the likelihood of successful outcomes.
Additionally, cellular therapy can potentially address previously untreatable or difficult-to-treat conditions. By focusing on the root cause of the disease and promoting natural healing, cellular therapy offers new hope for patients who have exhausted conventional treatment options. Moreover, it can potentially reduce the need for invasive surgeries and lifelong dependency on medication, improving the overall quality of life for patients.
Conclusion
In conclusion, cellular therapy represents a remarkable advancement in medical science, offering a new frontier of treatment possibilities. By harnessing the power of cells, this innovative approach has the potential to transform the lives of countless individuals suffering from various orthopedic conditions. With ongoing research and advancements, cellular therapy holds promise for the future of healthcare, providing hope for individuals seeking more effective and personalized treatment options.
San Diego Orthobiologics Medical Group is a leading provider of cellular therapy for the relief of arthritis, chronic tendon injuries, and other orthopedic conditions. Our treatment plans typically involve other forms of therapy to maximize improvements in biomechanics, fitness, nutritional status and healing capacity.