Nov 6, 2020
The human spine is composed of 24 individual bones called the vertebrae. In between these bones are the intervertebral discs, which are gel filled structures that act as shock absorbers. They consist of a tough outer layer called the annulus fibrosus that protects the disc’s gel-like interior, the nucleus pulposus. In the lower back, the discs are a little more than a third of an inch (10 millimeters) thick and about 1.5 inches (four centimeters) in diameter.[i]
A bulging disc or herniated disc occurs when the outer layer of the disc weakens and tears. This can cause the inner gel to bulge out to the spinal canal and affect the nearby nerves causing back pain, leg pain or muscle spasm. The disc tear can also cause leakage of materials into the spinal canal that can cause inflammation and pain.
Herniated discs most often occur in the lower back but can occur anywhere in the spine, including the neck and the midback. The location of the herniated disc often determines where the patient will feel symptoms of pain, tingling, numbness or weakness. Bulging discs in the lumbar spine can result in pain in the low back, buttocks, thighs, legs and feet. On the other hand, if your herniated disc is in the cervical spine, pain can be felt in the neck, shoulders, arms and hands.
What Causes a Herniated Disc?
Disc herniation can occur due to injury or age-related wear and tear. As people age, the disc nucleus pulposus loses hydration, wears down and leads to degeneration. Other factors may increase the risk of developing a herniated disc. These include:
- Repetitive lifting, pulling, pushing, bending and twisting
- Genetics
- Increased height (tall people)
- Smoking (decreases blood supply to the disk leading to degeneration)
A thorough medical history and physical examination can lead to the diagnoses of disc herniation. An MRI of the spine is an imaging modality that reveals herniated discs and other structural abnormalities of the spine.
Treatment Options
The treatment for most cases of mild to moderate herniated discs involves conservative measures which include the following:
- Activity modification: Avoid repetitive twisting, bending or lifting. Do not sit or stand for extended periods of time.
- Physical therapy to strengthen your trunk, arm and leg muscles that support the spine.
- Medications: Anti-inflammatory medications such as ibuprofen or naproxen, muscle relaxers, or pain killers
- Ice packs or heating pads
- Alternative therapies such as acupuncture, massage or gentle chiropractic manual therapies to manage pain.
Non-Surgical Interventions
When conservative measures fail to provide symptomatic relief, a board-certified spine specialist can offer injection treatments that do not require hospitalization and provide a more rapid recovery than surgery.
Epidural corticosteroid injection is a treatment that delivers steroid, a powerful anti-inflammatory medication, directly to the source of pain. This is performed using fluoroscopic (x-ray) guidance. This treatment can provide immediate relief of pain. The number of treatments is limited as repetitive steroid use could result to tissue damage, hormonal irregularities, osteoporosis and decreased immune response.
Cell-based therapies can treat disc degeneration and tears that are traditionally managed with medications or surgery. These treatments have been shown to increase disc hydration and disc cell proliferation, decrease inflammation, increase disc support tissue and assist in tissue healing. These therapies involve obtaining the patient’s own healthy cells and delivering them to the injured disc where they can jump start the body’s own regenerative healing processes.
- Platelet Rich Plasma uses platelets in the blood that release growth factors and proteins to promote tissue repair, while the plasma carries the hormones, electrolytes and nutrients required to nourish cells during the healing process.
- Cell Based Therapies use cells derived from the patient’s own bone marrow. Bone marrow contain adult stem cells that have the unique ability to develop into the specific kind of cells, including anulus and nucleus pulposus cells. They also contain many other healing cells and molecules that direct other cells in the area to form new blood vessels, awaken stem cells and produce collagen or other proteins essential for creating healthy new tissue.
Patients considering regenerative treatments such as these cell therapies need to know that the U.S. Food and Drug Administration (FDA) does not currently allow the use of stem cells derived from birth tissue products such as amniotic fluid or umbilical cord blood to treat orthopedic conditions. These donor products do not contain live stem cells and have not been tested for safety or efficacy.
Candidates for Cell-Based Therapies for Herniated Discs
The success of cell-based treatments for herniated discs is dependent upon the severity of your condition and your overall health. Cell-based treatments are not suitable for those who have active cancer, infection, history of blood disease, or are pregnant.
Cell-based therapies are giving new hope for long-lasting pain relief to many patients with injured discs. It is important that you take an active role in your healing and recovery with good nutrition and a commitment to overall fitness to achieve the best outcome.
Drs. Christopher J. Rogers and Mary A. Ambach of San Diego Orthobiologics Medical Group together have successfully treated thousands of patients with interventional spine procedures and cell-based treatments for more than three decades. They are published authors and cell therapy researchers. Their facility in Carlsbad contains the most advanced Regenerative Medicine technology in San Diego and offers same- day treatments with the highest level of safety and efficacy.
[i] https://www.kenhub.com/en/library/anatomy/the-intervertebral-discs
https://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/syc-20354095

Oct 27, 2020
On November 18th from 12:00 -1:00 pm PT, Dr. Chris Rogers and Dr. Mary A. Ambach will present on cell-based therapies.
Webinar on Non-Surgical Treatment Options for Osteoarthritis
Join our free webinar to learn about innovative Cell based therapies as a non-surgical treatment option for osteoarthritis and other orthopedic conditions.
Click HERE to register for the webinar!
Dr. Mary Ambach specializes in non-surgical orthopedics, regenerative therapies, and interventional pain management. As a key thought leader in the field of Regenerative Medicine, Dr. Ambach conducts research, trains physicians, and lectures at international medical conferences.
Dr. Christopher Rogers is one of the world’s leading experts in orthopedic regenerative medicine and a renowned speaker at national medical conferences. He has developed new approaches for the treatment of tendon injuries, osteoarthritis, and disc degeneration which provide a safe and viable alternative to surgery.

Oct 23, 2020
Regenerative medicine represents a complete breakthrough in modern medicine. The body’s ability to heal itself naturally is actually not a new thing. A fractured bone will regrow and heal the break. Cut yourself shaving, and the skin will heal. There are many examples of our body’s innate ability to heal injuries.
Now modern science and technology are now enabling physicians to help their patients discover new ways in which the body can heal itself. Within the specialty of orthopedics, regenerative medicine is offering healing and pain relief to patients who suffer from conditions such as osteoarthritis, herniated discs or ligaments and tendons injuries.
Orthobiologics Can Boost the Body’s Own Natural Healing Abilities
Orthobiologics are cells and substances derived from cells that are naturally found in your body. By concentrating them and delivering them to the site of injury, they can help speed up the healing process.
Here’s how it works:
When you injure a bone, muscle or tendon, the platelet cells in the blood are the first responders arriving on the scene to quickly start healing. White blood cells also rush to the injury site to ward off infection, control inflammation and become the clean-up crew [i]. Other important cells like stem cells participate in this complex symphony of repair. Specialists in orthopedic regenerative medicine can now boost these natural processes through several specialized treatments that help maximize the body’s own innate healing capabilities.
Regenerative Treatments for Orthopedic Conditions
There are different orthobiologic treatments that your regenerative medicine specialist can recommend depending on your orthopedic condition:
· Platelet Rich Plasma puts the healing properties of the patient’s own blood to work to repair damaged joints, tendons and muscles. The platelets in the blood release growth factors and proteins that promote tissue repair, while the plasma carries the hormones, electrolytes and nutrients required to nourish cells during the healing process. PRP treatments are customized to the particular individual and their injury in order to be most effective.
· Cell based therapies use cells derived from the patient’s own bone marrow or adipose (fat) tissue. These cells include adult stem cells and many other healing cells. They produce molecules that direct neighboring cells in the area to form new blood vessels, decrease inflammation and encourage formation of new healthy tissues. Stem cells are special cells that have the unique ability to develop into the specific kind of cell needed, whether that be a tendon, ligament, cartilage or bone cell. Skilled regenerative medicine practitioners use highly specialized processes to prepare these cells that are then delivered directly to the injured area to stimulate healing.
· Prolotherapy (Proliferative Therapy) uses dextrose and other natural substances that are injected into a chronically injured ligament, tendon, nerves or joint in order to help the body jump-start its own natural healing response.
Beware of Imposters
As regenerative treatments have become more widely recognized for their ability to address orthopedic conditions and the chronic pain associated with it, more and more clinics are trying to get in on the action.
If you are considering regenerative treatments for pain related to osteoarthritis, tennis elbow, degenerative discs in the spine or other conditions, you should perform due diligence on the clinic that offers it. The source, processing and delivery of the regenerative materials are critical to the success of the treatment.
Currently, the U.S. Food and Drug Administration (FDA) does not allow the use of stem cells derived from birth tissue products (amniotic fluid and tissue, umbilical cord blood) to treat orthopedic conditions because these donor products have not been proven to be safe or effective. Our board-certified specialists only use your own cells (autologous) to treat orthopedic conditions.
Maximizing the effectiveness of these treatments requires a state-of-the-art facility and equipment, as well as knowledge and experience in fluoroscopic (x-ray) or ultrasound guidance to ensure targeted delivery of the healing cells to the injured area.
Orthobiologic treatments that capitalize on the body’s own natural healing abilities is one of the most exciting opportunities in modern medicine to address and resolve the chronic pain associated with orthopedic conditions that affects millions of Americans.
Drs. Christopher J. Rogers and Mary A. Ambach of San Diego Orthobiologics Medical Group together have successfully treated thousands of patients with cell based therapies for more than three decades. They are published authors and cell therapy researchers. Their facility in Carlsbad contains the most advanced Regenerative Medicine technology in San Diego and offers same day treatments with the highest level of safety and efficacy.
[i] https://www.aarp.org/health/alternative-medicine/info-11-2008/super_healing.html
[ii] https://orthoinfo.aaos.org/en/treatment/helping-fractures-heal-orthobiologics/

Oct 9, 2020
The old adage among athletes is “No pain, no gain.” Sure, sore muscles after a hard workout are to be expected, but according to the National Safety Council, sports-related exercise accounted for nearly 800,000 injuries among adults in 2017.
These included injuries sustained from:
- Cycling
- Exercise with equipment
- Racket sports
- Recreational basketball
- Softball
- Soccer
- Swimming
Post-exercise soreness can occur up to 1-2 days after an exercise. However, if severe pain occurs during the exercise or immediately after, and if it progressively worsens and limits daily activities, you should seek consultation for a possible injury.
Breakthrough Options for Treating Sports Injuries
Regenerative medicine specialists can offer a number of options to treat sports-related injuries such as:
- Bursitis
- Tennis elbow
- Golfer’s elbow
- Tendinitis, Tendon tears, such as rotator cuff tears
- Hip and shoulder labral tears
- Ligament tears
- Meniscus tears
- Osteoarthritis
- Plantar fasciiosis
- Repetitive stress injuries
How Regenerative Medicine Treats Sports Injuries
Regenerative medicine uses state-of-the-art technology to maximize your body’s innate healing capacity. It uses your own cells to treat injuries in the joint cartilage, tendons or ligaments.
- Cell based treatments use cells derived from your own bone marrow or adipose (fat) tissue. These tissues contain adult stem cells and many other healing cells. When they are reinjected into an injured area they initiate healing. These cells produce molecules that direct cells to form new blood vessels, reduce inflammation, stimulate stem cells and encourage the formation of healthy tissue.
- Platelet Rich Plasma puts the healing properties of your own blood to work to heal damaged joints, tendons and muscles. Platelet cells from the blood release growth factors and proteins that promote tissue repair. The plasma carries hormones, electrolytes, proteins and nutrients that nourish cells during the healing process. PRP is not a “one-size-fits-all” treatment. To be effective, these treatments are customized to your specific medical condition. When performed correctly, PRP can bring pain relief and healing of injuries such as tennis elbow, tendon tears and osteoarthritis within weeks.
- Prolotherapy also known as Proliferative Therapy uses dextrose solutions and other natural substances to stimulate a healing response in chronically injured ligament, tendon or joints. The treatment can strengthen ligaments, improve stability and relieve pain. Scientific studies have demonstrated prolotherapy can be effective in treating tendinopathy, ligament sprains, tennis elbow, joint laxity, plantar fasciitis and osteoarthritis.
The “X” Factors
Great athletes are often said to possess the “X” factor, that special variable that influences successful outcomes. The same can be said of regenerative medicine treatments. The most successful regenerative treatments have the following “X” factors:
- Autologous source: Regenerative products that come from your own body (autologous) have been proven to be safe and effective in peer-reviewed research. The U.S. Food and Drug Administration (FDA) currently does not allow the use of donor stem cell products derived from amniotic fluid or other fetal tissues to treat orthopedic conditions. These products pose a risk of disease transmission or immune reaction. Moreover, these donor tissues do not to contain living stem cells, as opposed to what is claimed by the companies that market these products.
- Customized treatment: The best outcomes occur when your own cells and platelet rich plasma are prepared using the most advanced protocols to create a treatment that is customized to your specific injury.
- Targeted delivery: To maximize effectiveness, these regenerative treatments should be delivered under image guidance with fluoroscopy (x-ray) or ultrasound to ensure precise delivery to the injured area. Only physicians with fellowship training in advanced image guided procedures are certified to perform these procedures.
- Expert physicians: If you are considering regenerative medicine for the treatment of your spine or joint condition, seek a board certified physician who specializes in treating orthopedic injuries and has advanced training in regenerative medicine. These physicians are best suited to obtain the best results employing the latest research, technology and safety protocols.
Drs. Christopher J. Rogers and Mary A. Ambach of San Diego Orthobiologics Medical Group together have successfully treated thousands of patients with PRP and cell-based therapies for more than three decades. They are published authors and stem cell researchers. Their facility in Carlsbad contains the most advanced Regenerative Medicine technology in San Diego and offers same day treatments with the highest level of safety and efficacy.
https://www.iii.org/fact-statistic/facts-statistics-sports-injuries#:~:text=Basketball%20followed%20with%20about%20500%2C000,players%20have%20generated%20national%20headlines.
Oct 8, 2020
Join our free webinar to learn about PRP, an innovative non-surgical treatment option for osteoarthritis and other orthopedic conditions.
Dr. Mary Ambach specializes in non-surgical orthopedics, regenerative therapies, and interventional pain management. As a key thought leader in the field of Regenerative Medicine, Dr. Ambach conducts research, trains physicians, and lectures at international medical conferences.
Dr. Christopher Rogers is one of the world’s leading experts in orthopedic regenerative medicine and a renowned speaker at national medical conferences. He has developed new approaches for the treatment of tendon injuries, osteoarthritis, and disc degeneration which provide a safe and viable alternative to surgery.
Sep 30, 2020
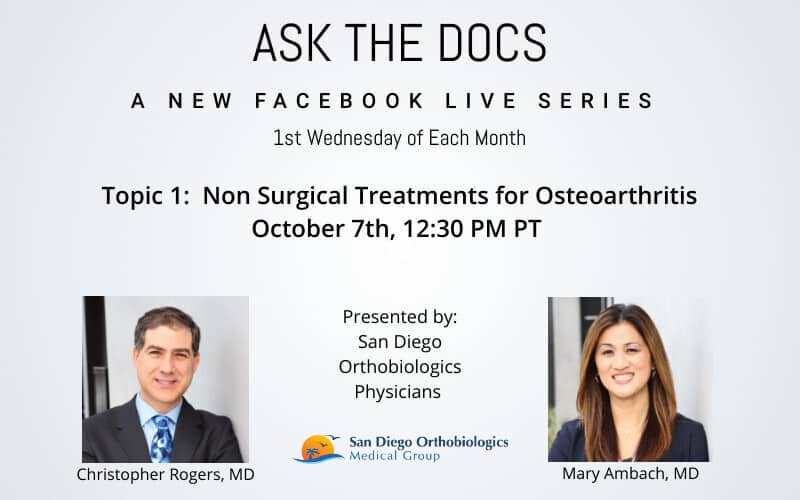
When: Wednesday, October 7, 2020
Time: 12:30 pm PST
Join the Facebook Live Event here
“Non Surgical Treatments for Osteoarthritis” Presented by Dr. Christopher Rogers and Dr. Mary A. Ambach
Join the first of our Free Facebook Live Series called Ask the Docs. In this first topic, SDOMG physician experts will answer your questions related to osteoarthritis and discuss non-surgical treatments in Regenerative Medicine and orthobiologics.
Your hosts:
Dr. Mary Ambach specializes in non-surgical orthopedics, regenerative therapies, and interventional pain management. As a key thought leader in the field of Regenerative Medicine, Dr. Ambach conducts research, trains physicians and lectures at international medical conferences.
Dr. Christopher Rogers is one of the world’s leading experts in orthopedic regenerative medicine and a renowned speaker at national medical conferences. He has developed new approaches for the treatment of tendon injuries, osteoarthritis and disc degeneration which provide a safe and viable alternative to surgery.
Stay Connected with SDOMG on Facebook