Feb 6, 2026
Joint preservation focuses on protecting and maintaining the natural function of joints for as long as possible. Instead of immediately resorting to joint replacement surgery, joint preservation aims to slow or halt joint degeneration, reduce pain, and improve mobility through early diagnosis and targeted treatments.
As arthritis and joint degeneration often develop gradually, early intervention plays a critical role in maintaining joint health. By addressing symptoms and structural changes early, patients may be able to delay—or even avoid—the need for surgical joint replacement.
What Causes Early Joint Degeneration?
Joint degeneration can occur for several reasons, and it often begins long before noticeable symptoms develop. Some of the most common contributing factors include:
- Osteoarthritis: The most common form of arthritis caused by wear and tear of cartilage.
- Previous Injuries: Sports injuries, ligament tears, fractures, or joint dislocations can accelerate degeneration.
- Repetitive Stress: Jobs or activities that place consistent strain on joints may lead to early damage.
- Inflammatory Conditions: Rheumatoid arthritis and other autoimmune diseases can affect joint tissues.
- Age and Genetics: Natural aging and family history both play a role in joint health.
- Excess Weight: Additional body weight places increased pressure on weight-bearing joints such as the knees and hips.
Understanding the underlying cause helps healthcare providers create a personalized joint preservation plan.
Recognizing Early Signs of Arthritis
Early arthritis symptoms can be subtle and are sometimes mistaken for normal aging or minor injury. Seeking medical evaluation when symptoms first appear can significantly improve treatment outcomes.
Common early warning signs include:
- Joint stiffness, especially in the morning or after inactivity
- Mild but persistent joint pain
- Swelling or tenderness around joints
- Decreased range of motion
- Clicking, grinding, or popping sensations in the joint
- Fatigue or discomfort during physical activity
If these symptoms persist or worsen over time, early intervention may help protect the joint from further deterioration.
Diagnostic Tools for Early Arthritis Detection
Accurate diagnosis is essential for effective joint preservation. Providers may use a combination of evaluation methods, including:
Physical Examination
Assessment of joint movement, stability, strength, and areas of pain.
Imaging Studies
- X-rays: Identify bone changes and cartilage loss.
- MRI: Detect soft tissue damage, cartilage injuries, and early joint degeneration.
- Ultrasound: Evaluate inflammation, fluid buildup, and soft tissue abnormalities.
Laboratory Testing
Blood tests may help identify inflammatory or autoimmune causes of joint pain.
Non-Surgical Joint Preservation Treatments
Many early arthritis cases can be managed effectively without surgery. Treatment plans often include a combination of therapies tailored to the patient’s condition and lifestyle.
Physical Therapy and Rehabilitation
Targeted exercises help strengthen muscles around the joint, improve flexibility, and enhance stability, which reduces strain on damaged joint structures.
Activity Modification
Adjusting daily activities or athletic movements can reduce repetitive joint stress while maintaining overall mobility and function.
Weight Management
Maintaining a healthy weight can significantly reduce pressure on joints, particularly in the knees, hips, and spine.
Medication Management
Anti-inflammatory medications and pain relievers may help control symptoms and improve comfort during daily activities.
Advanced Joint Preservation Procedures
When conservative treatments are not enough, minimally invasive and regenerative therapies may help support joint repair and healing.
Injection-Based Therapies
- Corticosteroid Injections: Reduce inflammation and provide temporary pain relief.
- Hyaluronic Acid Injections: Improve joint lubrication and mobility.
- Platelet-Rich Plasma (PRP): Uses the patient’s own blood components to promote healing and tissue repair.
Regenerative Medicine
Emerging regenerative therapies aim to stimulate the body’s natural healing processes to repair damaged tissues and slow joint degeneration.
Minimally Invasive Arthroscopic Procedures
In some cases, arthroscopy may be used to repair cartilage, remove damaged tissue, or correct joint alignment before advanced arthritis develops.
Lifestyle Strategies to Support Joint Preservation
Patients can play an active role in maintaining joint health through daily habits that support long-term mobility.
Helpful strategies include:
- Staying physically active with low-impact exercises such as swimming, cycling, or walking
- Practicing stretching and flexibility routines
- Using proper body mechanics during lifting or exercise
- Wearing supportive footwear
- Following an anti-inflammatory diet rich in whole foods, lean proteins, fruits, vegetables, and healthy fats
When Is Joint Replacement Necessary?
Joint replacement surgery may become necessary when:
- Joint damage is severe
- Pain significantly limits daily activities
- Conservative treatments no longer provide relief
- Mobility and quality of life are severely affected
The goal of joint preservation is not to eliminate joint replacement entirely but to delay it whenever possible, allowing patients to maintain their natural joint function longer.
The Importance of Early Arthritis Care
Early arthritis care focuses on proactive management rather than reactive treatment. Patients who seek evaluation and treatment at the first signs of joint discomfort often experience better outcomes, slower disease progression, and improved quality of life.
Healthcare providers specializing in joint preservation can develop personalized treatment plans designed to:
- Reduce inflammation and pain
- Improve joint stability and function
- Slow or prevent further joint damage
- Support long-term mobility and activity levels
Final Thoughts
Joint preservation and early arthritis care emphasize the importance of early diagnosis, conservative treatment, and proactive lifestyle changes. With modern medical advancements and individualized care plans, many patients can successfully manage arthritis symptoms and maintain active, healthy lives without immediate surgery.
If you are experiencing early joint pain, stiffness, or mobility limitations, seeking professional evaluation can help protect your joints and preserve long-term function.
Dec 12, 2025
Joint degeneration doesn’t happen overnight. It’s a slow, progressive process — but the earliest warning signs are often subtle enough that many people shrug them off as “getting older” or “overdoing it.” Identifying these changes early can make all the difference in treatment outcomes, mobility, and long-term joint health. And thanks to advances in regenerative medicine, patients now have powerful options that can protect, repair, and even restore damaged tissue before the problem becomes severe.
Below, we break down the early symptoms to watch for and explore how modern regenerative therapies can help interrupt the degenerative cascade.
What Early Joint Degeneration Looks Like
1. Persistent Morning Stiffness
If you feel “rusty” or tight first thing in the morning — especially in the knees, hips, or spine — this can indicate early cartilage wear or inflammation. Stiffness that improves as you move around is a classic hallmark of early degenerative changes.
2. Clicking, Popping, or Grinding
Noisy joints aren’t always dangerous, but when those sounds are paired with discomfort, swelling, or instability, they may signal roughened surfaces or early cartilage breakdown.
3. Pain With Activity That Improves With Rest
You might feel fine at rest but experience dull aching during:
- Walking up or down stairs
- Long periods of standing
- Squatting or lifting
- High-impact workouts
This “use-related pain” often shows up years before advanced arthritis.
4. Swelling or Warmth Around the Joint
Mild inflammation is one of the earliest internal reactions to joint stress or degeneration. Even occasional swelling after activity can indicate chronic irritation inside the joint.
5. Reduced Range of Motion
Maybe your knee doesn’t bend the way it used to, or your shoulder feels tight when reaching overhead. Loss of flexibility is often one of the first measurable signs of joint deterioration.
6. Fatigue or Weakness in the Joint
Muscles surrounding a degenerating joint often work overtime to compensate, which can create fatigue, shakiness, or weakness during routine tasks.
Why Early Action Matters
Once cartilage has worn away significantly, it cannot regenerate on its own — and late-stage arthritis often requires aggressive treatments like joint replacement. Early intervention, however, can slow or even stop the degenerative cycle. The goal is to reduce inflammation, restore stability, and stimulate natural repair pathways before more permanent damage occurs.
This is where regenerative medicine shines.
How Regenerative Therapies Can Help
Platelet-Rich Plasma (PRP)
PRP concentrates your body’s own growth factors to:
- Reduce inflammation
- Promote tissue repair
- Slow cartilage breakdown
- Improve joint lubrication
Great for early osteoarthritis, tendon irritation, and chronic joint strain.
Orthobiologics
These treatments use biologically active cells and proteins to enhance healing in damaged tissue. Orthobiologics can improve structural stability, reduce inflammation, and support long-term joint health.
Cell–Based Therapies
These therapies may help stimulate new tissue formation in joints that show early degenerative changes. They can support:
- Cartilage protection
- Improved mobility
- Reduced pain
- Enhanced shock absorption
Especially useful for knees, hips, shoulders, and spine-related degeneration.
Hyaluronic Acid (Viscosupplementation)
A lubrication-boosting gel injected into the joint to:
- Improve glide
- Reduce pain
- Support smoother movement
Works well for mild to moderate osteoarthritis.
Lifestyle + Regenerative = Long-Term Prevention
The best outcomes happen when regenerative therapies are paired with:
- Strength training
- Weight management
- Physical therapy
- Anti-inflammatory nutrition
- Activity modification
Together, these strategies help reinforce joint support structures and reduce ongoing stress.
When to Seek Evaluation
You don’t need severe pain to justify seeing a specialist. In fact, the sooner you understand what’s happening inside your joints, the more options you have to preserve their health.
Seek evaluation if you notice:
- Recurring stiffness
- Activity-related pain
- Early swelling
- Clicking or grinding
- Weakness or instability
A simple exam — sometimes paired with X-ray or ultrasound — can determine your level of joint degeneration and whether regenerative therapies are appropriate.
Final Thoughts
Joint degeneration doesn’t have to be inevitable or irreversible — especially when it’s caught early. Modern regenerative options offer patients a chance to protect and restore joint health naturally, often delaying or avoiding more invasive procedures down the line.
If you’re starting to notice the early signs, now is the perfect time to explore your options and take proactive steps to keep your joints strong, mobile, and pain-free for years to come.

Dec 5, 2025
As temperatures drop, many people notice their joints becoming stiff, achy, or more painful than usual. Winter weather can aggravate conditions like arthritis, tendon injuries, and chronic joint degeneration—making it harder to stay active and comfortable. While traditional treatments such as NSAIDs, bracing, and heat therapy offer temporary relief, patients looking for longer-term improvement often turn to regenerative medicine.
Here’s why winter is actually one of the best times to explore regenerative options like PRP (platelet-rich plasma), orthobiologics, and cell-based therapies.
Why Joints Hurt More in Winter
Many patients describe their joints as “weather predictors,” especially when cold air arrives. Several factors explain why winter intensifies joint discomfort:
1. Changes in Barometric Pressure
Dropping pressure can cause joint tissues to expand slightly, leading to increased stiffness or pain—especially in joints already affected by inflammation or degeneration.
2. Cold Muscles = Stiffer, Tighter Movement
Cold temperatures reduce muscle elasticity. This places extra strain on tendons, ligaments, and joints.
3. Reduced Activity Levels
Shorter days and cold weather reduce physical activity, which weakens supportive muscles and worsens joint mobility.
4. Increased Inflammation
For some individuals, cold stress increases inflammatory responses, intensifying pain in arthritic or injured joints.
Why Winter Is a Smart Time to Choose Regenerative Medicine
Regenerative therapies work by supporting the body’s natural ability to repair and restore damaged tissues. During the winter, this approach can be particularly beneficial for several reasons.
1. Winter Often Marks a Natural Slowdown—Perfect for Recovery
Many people slow their routines during the colder months. This makes it easier to schedule the brief downtime required after regenerative injections.
2. Reduced Activity Helps Regeneration Work Better
After treatments like PRP, patients need a window of lower impact activity. Winter’s pace naturally aligns with this healing phase.
3. Get Ahead of Spring Activity
Whether you’re preparing for gardening, sports, travel, or outdoor activities, winter treatment gives your joints time to heal so you can be more active (and pain-free) when spring arrives.
4. Regenerative Medicine Addresses the Root Cause
Unlike medications that only mask pain, regenerative therapies aim to:
- reduce inflammation
- improve blood flow
- support tissue repair
- slow or reverse degenerative processes
This makes it an ideal option for chronic winter flares.
5. Less Reliance on Seasonal Pain Medications
Patients often notice increased medication use during colder months. Regenerative care can help reduce dependence on pills or repetitive steroid injections.
Common Joint Issues Treated with Regenerative Therapy in Winter
Winter pain tends to flare in:
- knees (arthritis, meniscus issues, cartilage loss)
- hips (labral tears, early arthritis)
- shoulders (rotator cuff injuries, tendonitis)
- elbows (tendon degeneration)
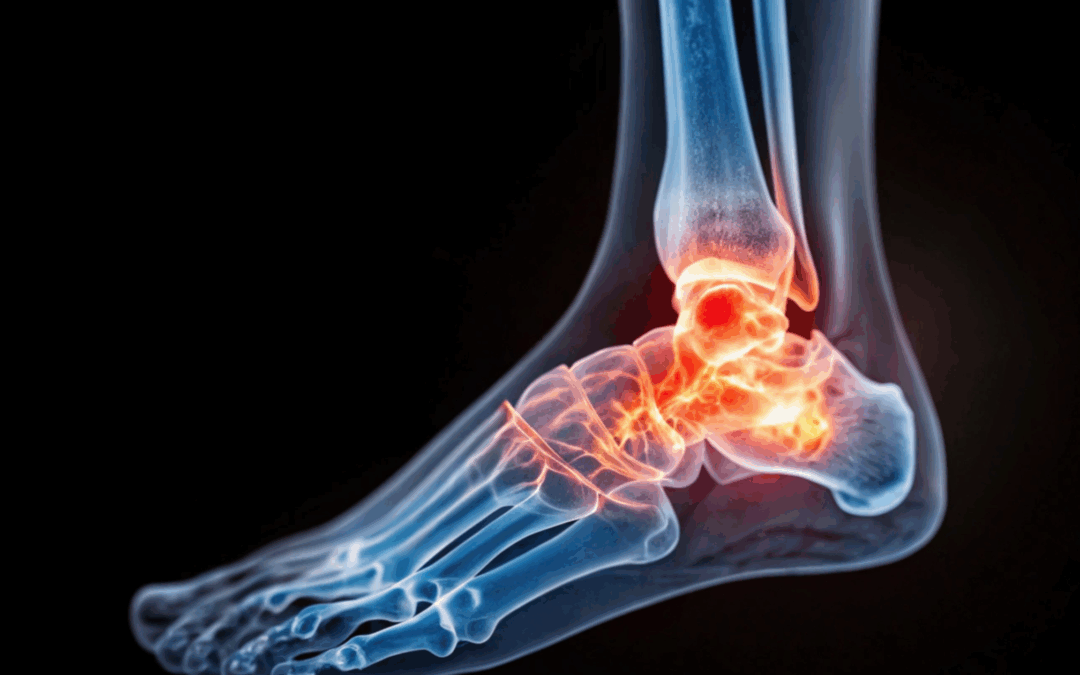
- ankles and feet (Achilles issues, plantar fasciitis)
- spine joints (facet arthritis)
Regenerative medicine helps stabilize and strengthen these areas while reducing pain.
Types of Regenerative Treatments That Work Well in Winter
PRP Injections (Platelet-Rich Plasma)
Uses your own platelets to decrease inflammation and stimulate tissue repair.
Orthobiologics
Includes growth-factor-rich injections, micro-fat grafting, and other biologic agents that support healing.
Cell-Based Therapies
Derived from bone marrow or fat tissue to promote repair in more advanced degeneration.
Your provider will recommend options based on imaging, severity, and your activity goals.
Supporting Joint Care Through the Cold Season
Regenerative medicine works best when paired with targeted lifestyle strategies. Consider adding:
- winter-appropriate movement (indoor walking, stretching, low-impact exercise)
- anti-inflammatory nutrition
- joint-warming routines (heat therapy, warm showers before activity)
- physical therapy for mobility and strength
- proper winter footwear and traction
These habits help maintain the benefits of regenerative treatment and keep winter symptoms under control.
Is Regenerative Medicine Right for You This Winter?
If cold weather consistently makes your joint pain worse—or if you’re tired of managing symptoms year after year—this may be the perfect time to explore regenerative options. These treatments are especially helpful if:
- conservative therapies have stopped working
- pain interferes with winter activity
- you want a longer-term, non-surgical approach
- you prefer natural healing over medications
- you want to prepare your body for an active spring
Winter doesn’t have to be painful. With the right regenerative plan, you can stay mobile, reduce inflammation, and give your joints the healing support they need.
Oct 17, 2025
Joint pain often starts subtly — a little stiffness in the knees, soreness in the shoulders, or discomfort after activity. These are often signs of early joint degeneration, when cartilage and surrounding tissues begin to wear down. Fortunately, regenerative medicine offers new hope for restoring joint health before these early issues turn into chronic pain or arthritis.
Understanding Early Joint Problems
Our joints are built to move smoothly, cushioned by cartilage, lubricated by joint fluid, and supported by strong ligaments and tendons. Over time, however, wear and tear, injury, or inflammation can damage these structures.
Early joint problems may include:
- Mild stiffness or aching after activity
- Pain when bending or climbing stairs
- Swelling or tenderness around the joint
- Decreased flexibility or “creaking” sensations
At this early stage, the joint still has the potential to heal — especially with regenerative treatments that help the body repair and rebuild healthy tissue.
How Regenerative Medicine Works
Regenerative medicine focuses on stimulating the body’s natural healing processes. Rather than just masking symptoms with medication or injections, regenerative therapies aim to restore tissue health, reduce inflammation, and improve joint function.
These treatments use the body’s own biological materials — like platelets or stem cells — to encourage tissue repair and regeneration where it’s needed most.
Common Regenerative Treatments for Early Joint Damage
1. Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves concentrating platelets from your own blood and injecting them into the affected joint. These platelets contain powerful growth factors that:
- Stimulate tissue repair
- Reduce inflammation
- Promote collagen and cartilage regeneration
PRP can be used for early joint problems in the knees, shoulders, hips, or other joints — helping restore comfort and mobility naturally.
2. Stem Cell Therapy
Stem cell therapy introduces healing cells — usually derived from bone marrow or adipose (fat) tissue — into the damaged joint. These cells can help rebuild cartilage, improve cushioning, and restore balance within the joint environment.
Early research suggests stem cell therapy may slow or even reverse early degenerative joint changes, helping patients avoid or delay more invasive procedures like joint replacement.
3. Prolotherapy
Prolotherapy uses a natural dextrose-based solution injected around weakened ligaments and tendons to trigger the body’s repair response. This mild inflammation promotes the growth of stronger connective tissue, improving joint stability and function.
Over time, this can reduce pain caused by instability or early joint wear.
Benefits of Early Regenerative Intervention
Addressing joint problems early can prevent more serious degeneration and preserve mobility. The benefits of regenerative therapies include:
- Minimally invasive procedures with little to no downtime
- Reduced need for pain medications or steroids
- Improved joint strength and flexibility
- Potential long-term relief by promoting true healing rather than masking symptoms
Is Regenerative Treatment Right for You?
Regenerative therapies may be ideal if you’re experiencing mild to moderate joint pain, early arthritis, or mobility issues that haven’t improved with rest, physical therapy, or standard treatments.
A pain management or orthopedic specialist can evaluate your condition through imaging and examination to determine whether PRP, stem cell therapy, or prolotherapy is the right approach for your needs.
A Future-Focused Approach to Joint Care
Regenerative treatments are changing how we approach joint pain — emphasizing healing, repair, and long-term joint preservation. For those with early joint problems, these therapies offer a proactive, restorative way to protect joint health and maintain an active lifestyle.
If you’ve noticed stiffness or joint discomfort, now is the time to explore regenerative options. Early action can make all the difference in keeping your joints healthy and pain-free for years to come.
Jul 31, 2025
Tendon and ligament injuries are notoriously slow to heal, often sidelining athletes, workers, and everyday individuals for weeks or even months. While rest, physical therapy, and sometimes surgery are commonly prescribed treatments, many people overlook a crucial factor that can significantly influence recovery: nutrition.
Tendons and ligaments are made up of dense connective tissue primarily composed of collagen—a protein that gives these structures strength and flexibility. Because they have a limited blood supply, their healing process is slower compared to muscles or skin. However, by optimizing nutrition, you can give your body the essential building blocks it needs to repair and regenerate connective tissue more efficiently.
Understanding the Healing Process
When a tendon or ligament is injured—whether through a sprain, strain, or tear—the body initiates a complex healing response that unfolds in three phases:
- Inflammation (First few days) – The area becomes swollen and painful as the immune system clears damaged cells and begins tissue repair.
- Proliferation (Up to several weeks) – New collagen fibers are laid down to rebuild the injured tissue.
- Remodeling (Weeks to months) – Collagen is reorganized to restore strength and function.
Nutrition plays a key role in all three stages, supporting everything from reducing excessive inflammation to synthesizing new collagen.
Key Nutrients for Tendon and Ligament Repair
1. Protein and Amino Acids
Protein is the foundation of tissue repair. Amino acids like glycine, proline, and lysine are essential for collagen synthesis. A diet lacking in protein can significantly delay healing.
Best sources:
- Lean meats, poultry, fish
- Eggs
- Greek yogurt
- Bone broth (rich in collagen and gelatin)
- Plant-based sources like quinoa, lentils, and soy
2. Vitamin C
Vitamin C is a cofactor for collagen production and helps stabilize the collagen triple-helix structure. It also has antioxidant properties that protect healing tissues from oxidative stress.
Best sources:
- Citrus fruits (oranges, grapefruit)
- Strawberries
- Bell peppers
- Kiwi
- Broccoli
3. Zinc
Zinc plays a critical role in tissue regeneration, immune response, and collagen synthesis. Even a mild deficiency can impair healing.
Best sources:
- Pumpkin seeds
- Oysters
- Beef
- Chickpeas
- Cashews
4. Omega-3 Fatty Acids
These healthy fats help modulate the inflammatory response, reducing excessive inflammation that can hinder healing.
Best sources:
- Salmon and other fatty fish
- Chia seeds
- Walnuts
- Flaxseeds
- Fish oil supplements
5. Vitamin A
This fat-soluble vitamin helps with collagen formation and immune function. It’s also involved in cellular growth and differentiation, vital for tissue regeneration.
Best sources:
- Carrots
- Sweet potatoes
- Spinach
- Kale
- Liver
6. Copper and Manganese
These trace minerals are important co-factors in enzymatic reactions involved in collagen cross-linking, which strengthens connective tissue.
Best sources:
- Nuts and seeds
- Shellfish
- Whole grains
- Leafy greens
Collagen and Gelatin Supplements
There’s growing evidence that supplementing with hydrolyzed collagen or gelatin, especially when combined with vitamin C, can enhance tendon and ligament repair. These supplements provide key amino acids like glycine and proline in a readily absorbable form.
One study from the American Journal of Clinical Nutrition found that consuming gelatin before exercise increased collagen synthesis in ligaments. This is particularly helpful during the rehab phase of recovery when tissues are being remodeled and strengthened.
Pro tip: Take collagen or gelatin supplements about 30–60 minutes before physical therapy or light rehab exercises for optimal impact.
Anti-Inflammatory vs. Pro-Inflammatory Foods
While some inflammation is necessary for healing, chronic inflammation can interfere with recovery. Choosing the right types of foods can help modulate this response.
Eat more:
- Colorful vegetables and fruits
- Turmeric and ginger
- Green tea
- Healthy fats (olive oil, avocado)
Avoid or limit:
- Refined sugars
- Processed foods
- Fried foods
- Excessive alcohol
- Trans fats
Hydration and Connective Tissue Health
Tendons and ligaments require adequate hydration to maintain elasticity and function. Dehydrated tissues are more prone to injury and slower to repair.
Tips to stay hydrated:
- Drink water consistently throughout the day
- Include electrolyte-rich fluids (especially if sweating heavily)
- Limit caffeine and alcohol, which can dehydrate
Timing Your Nutrition
When you eat can also affect recovery. Aim to space protein-rich meals evenly throughout the day to promote continuous tissue repair. Pairing protein with antioxidant-rich vegetables helps reduce oxidative stress on healing tissues.
Additionally, nutrient timing around rehabilitation sessions—like consuming vitamin C and collagen beforehand—can enhance tissue remodeling.
Nutrition for Long-Term Tendon and Ligament Health
Even after recovery, maintaining a diet that supports connective tissue can help prevent future injuries. Consider these strategies:
- Continue regular intake of collagen-boosting nutrients
- Avoid crash diets that deprive the body of essential micronutrients
- Focus on maintaining muscle strength and joint mobility through consistent exercise
- Use anti-inflammatory foods as part of your daily diet
Conclusion
Nutrition is a powerful tool in the recovery journey from tendon and ligament injuries. While it won’t replace physical therapy or rest, the right nutrients can significantly accelerate healing and improve tissue strength. Whether you’re dealing with an acute injury or managing chronic connective tissue damage, paying attention to what’s on your plate can make a meaningful difference in how quickly—and how well—you recover.

Jul 16, 2025
Joint pain can creep in slowly or hit suddenly—but either way, it can impact your mobility, mood, and overall quality of life. Whether you’re dealing with age-related wear and tear, chronic inflammation, or recovering from an injury, adopting everyday habits that support joint health can make a world of difference. The good news? You don’t always need a prescription to find relief. A few simple lifestyle adjustments can go a long way in keeping your joints strong, flexible, and pain-free.
Here are natural, evidence-backed habits you can incorporate into your daily life to support your joints and reduce discomfort.
1. Keep Moving—But Move Smart
Movement is medicine for your joints. Staying active helps lubricate the joints, strengthen surrounding muscles, and maintain a healthy range of motion.
- Low-impact exercises like walking, swimming, biking, and yoga are excellent choices.
- Strength training helps stabilize joints and reduce stress on them.
- Stretching regularly keeps muscles flexible and reduces stiffness.
Tip: Avoid long periods of inactivity. If you sit at a desk, stand up and stretch every hour.
2. Maintain a Healthy Weight
Carrying excess weight puts unnecessary pressure on weight-bearing joints—especially the knees, hips, and lower back. In fact, for every extra pound you carry, your knees experience about four extra pounds of pressure.
- Shedding even 5–10% of your body weight can significantly reduce joint strain and pain.
- Focus on slow, sustainable weight loss through diet and exercise.
Bonus: Weight loss also lowers systemic inflammation, which can ease joint pain.
3. Prioritize Anti-Inflammatory Nutrition
What you eat has a direct impact on your inflammation levels and joint health. Incorporating anti-inflammatory foods can help reduce pain naturally.
- Foods to eat: Fatty fish (like salmon), leafy greens, berries, olive oil, turmeric, ginger, nuts, and seeds.
- Foods to limit: Sugar, red meat, processed snacks, and fried foods.
Tip: A Mediterranean-style diet is particularly joint-friendly.
4. Stay Hydrated
Cartilage—the flexible tissue that cushions your joints—is made mostly of water. Staying hydrated keeps this tissue lubricated and reduces friction during movement.
- Aim for at least 8–10 glasses of water per day, more if you’re active or in a hot climate.
- Herbal teas and water-rich fruits like watermelon and cucumber also count toward hydration.
Dehydration can cause joint stiffness and increased sensitivity to pain.
5. Support Your Joints with Supplements
Certain natural supplements have been shown to support joint health and reduce inflammation.
- Glucosamine and chondroitin: May help rebuild cartilage and reduce pain.
- Turmeric/curcumin: A powerful anti-inflammatory.
- Omega-3 fatty acids: Found in fish oil, these reduce inflammation system-wide.
- Collagen peptides: Support cartilage and connective tissue integrity.
Always consult your healthcare provider before starting a new supplement.
6. Use Proper Posture and Ergonomics
Slouching or using improper body mechanics can stress your joints over time. Make small adjustments to support joint alignment throughout the day.
- Sit with your back straight, feet flat on the ground, and shoulders relaxed.
- Use supportive chairs or standing desks as needed.
- When lifting objects, use your legs—not your back—and keep items close to your body.
Ergonomic tweaks at your workstation can prevent repetitive stress injuries.
7. Get Plenty of Restful Sleep
Quality sleep is essential for healing and reducing inflammation. During deep sleep, your body produces hormones that repair tissue and regulate immune response.
- Aim for 7–9 hours of sleep per night.
- Create a calming bedtime routine: turn off screens, dim the lights, and avoid caffeine late in the day.
- Consider supportive pillows or a mattress that helps align your spine and joints.
Poor sleep is linked to increased perception of pain and joint stiffness.
8. Manage Stress Effectively
Chronic stress triggers the release of cortisol, a hormone that can promote inflammation in the body. Reducing stress can ease both physical and emotional tension that often worsens joint pain.
- Try meditation, deep breathing exercises, journaling, or spending time in nature.
- Make time for hobbies, connection with others, and digital detoxes.
Mind-body practices like tai chi and yoga offer both physical and mental relief.
9. Avoid Smoking and Excess Alcohol
Smoking reduces blood flow to joints and damages connective tissue. Meanwhile, excessive alcohol can deplete your body of nutrients and contribute to inflammation.
- If you smoke, seek out resources to quit—it can significantly improve joint and overall health.
- Drink alcohol in moderation, if at all.
Small lifestyle changes add up over time—quitting smoking is one of the most impactful things you can do for joint health.
10. Listen to Your Body
One of the most underrated habits is simply tuning in to your body’s signals. If an activity causes joint pain or stiffness, it may be a sign you need rest or a modification.
- Alternate between activity and rest.
- Don’t push through sharp or persistent joint pain.
- See a healthcare provider if symptoms don’t improve or worsen.
Early intervention can prevent long-term joint damage.
Final Thoughts
You don’t need to overhaul your life to take better care of your joints. By adopting small, consistent habits—like staying active, eating anti-inflammatory foods, and managing stress—you can support your body’s natural ability to maintain strong, pain-free joints.
These habits are powerful on their own but even better when practiced together. Start with one or two changes today and build on your progress each week. Your joints will thank you for years to come.